Nerve Cell Injury and Chronic Inflammation Need Be Focus of ALS Research, Study Argues
The greater incidence of amyotrophic lateral sclerosis (ALS) among professional athletes and people with head trauma, and the faster functional decline seen in animal models after localized nerve injury, strongly suggests that nerve injury plays a role in initiating disease processes, a review study reported.
Needed avenues of future research include new animal models that better mimic such injury in this disease, more non-invasive biomarkers of disease progression, and studies on preventing nerve degeneration by targeting a factor important to nerve cells called neuregulin-1 (NRG1), its researchers wrote.
The review, “Disease propagation in amyotrophic lateral sclerosis (ALS): an interplay between genetics and environment,” was published in the Journal of Neuroinflammation.
Despite considerable research effort, ALS remains poorly understood, with no effective therapy.
Researchers at the University of Illinois at Chicago looked at mechanisms that might contribute to ALS, with a focus on “the possibility of injury as an instigating event, and the potential role of the growth factor neuregulin in disease spread,” they wrote.
Although ALS has a genetic component, they noted that the higher risk of this severe disease seen among veterans and athletes suggests nerve injury could play a key role.
Studies have reported that being physically active correlates with a higher risk of developing ALS. Evidence linking head trauma to the disorder’s onset also points toward the involvement of injury.
“Population studies show that the disease is 2–3 times more common in varsity and professional athletes and veterans, even without combat experience,” the researchers wrote.
One potential explanation is that injury to a nerve could trigger disease onset at that site. Other studies show conflicting results, however, suggesting that any role nerve injury might play could be complicated and difficult to unravel.
A Danish study, for instance, found that a person’s age (54 or younger) and the length of time between their injury and ALS diagnosis (more than five years) strongly affected their risk of developing the disorder.
Animal models provide several critical insights into the relationship between nerve injury and ALS, the research team wrote.
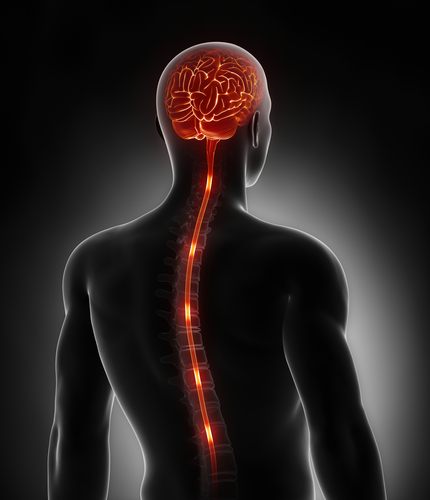
Studies using the mutant superoxide dismutase 1 (SOD1)-expressing mouse model have shown that a crushed sciatic nerve caused several ALS-like symptoms, and the loss of motor neurons in regions of the spinal cord.
The same mutation in rats, while leading to more variability in where symptoms first appear, added to the evidence linking nerve injury to ALS onset by also showing that a sciatic nerve crush injury hastened functional decline and led to shorter survival times.
The inflammatory response to nerve injury appears to be a main driver of neurodegeneration, the researchers wrote. During the normal injury repair process, specialized immune cells of the central nervous system called microglia are thought to modify synapses and recruit other immune cells to the sites of nerve injury.
But in ALS animal models, microglia show prolonged inflammatory responses followed by significant reductions in motor neurons, suggesting an active role of these immune cells in disease progression. Microglia carrying ALS mutations were also seen to exacerbate disease progression in these animals, while healthy microglial cells promoted survival.
“One issue that continues to plague ALS research is the lack of effective therapeutic translation from animal models to patients,” the researchers stated, while adding that “abnormal inflammation and microglial activation” is also seen in tissues taken from patients post-mortem.
Understanding how and when to lessen inflammatory responses will likely be vital to successful treatment efforts, they added.
One promising therapeutic target noted was the nerve growth and differentiation factor NRG1.
NRG1 is important for the growth and development of neuromuscular junctions — the sites where motor nerve cells and muscle fiber communicate — and to nerve injury repair. Prolonged and excessive signaling by NRG1, however, can lead to pathological inflammation by activating microglia.
NRG1 signaling does increase in ALS models, and studies that reduce microglial activity by blocking NRG1 after nerve injuries also lessen the development of chronic pain.
Researchers suggest that blocking NRG1-mediated neuroinflammation could prevent several of the effects that contribute to ALS progression, regardless of a patient’s underlying genetics.
They also suggest that new animal models in which nerve injury leads to ALS onset could prove useful in testing potential therapies, and that identifying more non-invasive biomarkers of ALS progression will be critical to developing such treatments.
“These key facets,” the investigators concluded, “will enable a better understanding of disease pathology and paradigm shifts in treatment, ultimately resulting in therapies truly capable of providing hope for patients.”