FAQs about types of ALS
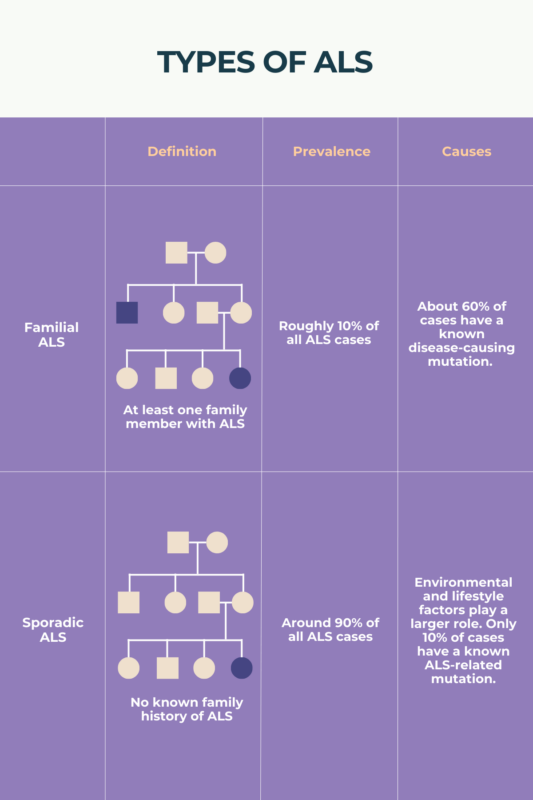
Amyotrophic lateral sclerosis (ALS) is usually classified in two ways: as either sporadic or familial, based on whether or not a patient has a family history of the disease, and as either limb-onset or bulbar-onset, depending on where in the body ALS symptoms first appear. The disease also may be further divided into more specific subtypes based on factors like the presence or absence of specific genetic mutations.
About 90% of people with amyotrophic lateral sclerosis (ALS) have sporadic disease, meaning that the affected individual does not have a family history of ALS. Another common type, affecting around two-thirds of patients, is limb-onset ALS, in which individuals first experience symptoms that affect muscles in the arms or legs.
Amyotrophic lateral sclerosis (ALS) is a progressive disorder marked by muscle weakness and atrophy (wasting), which usually is mild to start and affects only one body part, then becomes more severe and gradually spreads to impact the whole body. It is classified based on the presence or absence of a family history, as well as based on the first symptoms that develop. Because these are descriptors of the disease at its onset, ALS classifications generally do not change over time.
There can be a lot of variability in how amyotrophic lateral sclerosis (ALS) manifests and progresses, even among people who are classified as having the same type of ALS. In general, ALS disease progression is faster in bulbar-onset disease, where the first muscles affected are in the mouth and throat, compared with limb-onset disease, in which symptoms initially affect the arms or legs.
Amyotrophic lateral sclerosis (ALS), also called Lou Gehrig’s disease, is classified as familial or sporadic based on whether or not the affected individual has a family history of the disease. ALS also can be classified as limb-onset or bulbar-onset based on whether initial symptoms affect the limbs or the jaw and throat. Thus, doctors closely examine a person’s family history and clinical onset to determine which types of ALS a person has.
Related Articles

 Fact-checked by
Fact-checked by