FAQs about ALS diagnosis
Amyotrophic lateral sclerosis (ALS) can develop at any age, although it is more common with increasing age. The majority of patients are diagnosed between the ages 55 and 75, but there are reports of the disease being diagnosed in young children.
Symptoms of muscle weakness that get progressively worse over time characterize amyotrophic lateral sclerosis (ALS). In most patients, this weakness starts in the hands and/or feet on one side of the body before spreading elsewhere, though more rarely it can begin affecting the muscles around the mouth and throat. Signs such as unexplained difficulty with writing or carrying things, problems walking, or unexplained speech abnormalities may prompt a diagnostic workup for potential ALS.
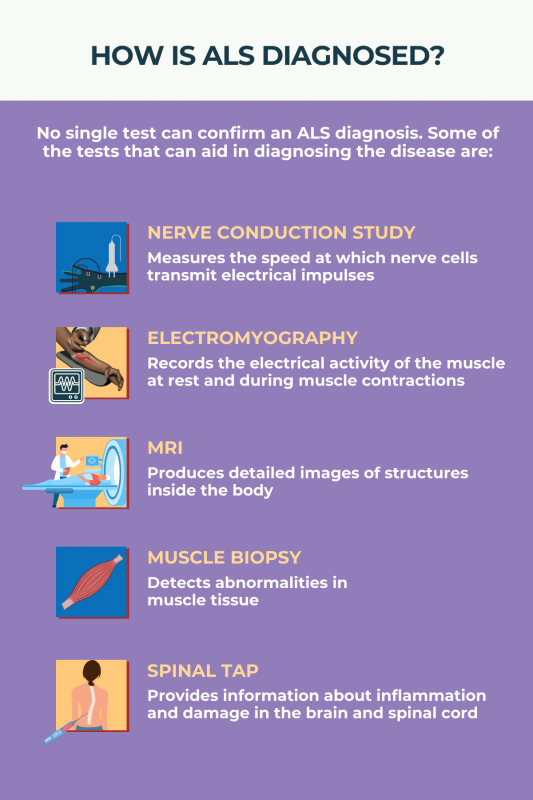
There is no single test that can diagnose amyotrophic lateral sclerosis (ALS). Instead, a diagnosis is made based on the combination of signs and symptoms indicative of the disease, together with tests to exclude other potential explanations for the symptoms. It’s common for a diagnostic evaluation for ALS to take several months; most people are diagnosed between 10 and 16 months after symptoms first appear.
Amyotrophic lateral sclerosis (ALS) is a progressive disorder, meaning it will get increasingly worse over time. Without a proper diagnosis, people with ALS cannot receive appropriate care, including treatments that may slow the progression of the disease.
Amyotrophic lateral sclerosis (ALS) is diagnosed via a combination of assessments that aim to identify disease-related damage to motor neurons that gets progressively worse over time. Diagnosis also involves tests to exclude other conditions that may cause similar symptoms.
Related Articles

 Fact-checked by
Fact-checked by