FAQs about ALS
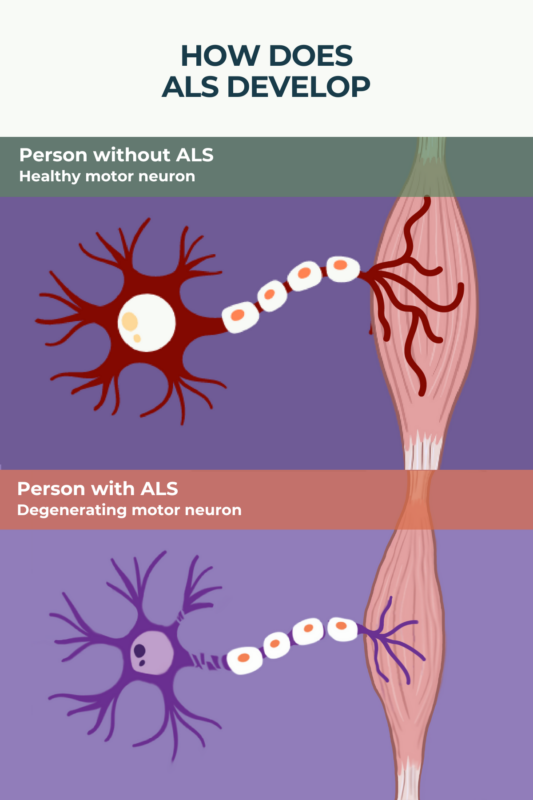
There’s no known exact cause of amyotrophic lateral sclerosis (ALS), but its symptoms are due to the progressive dysfunction and death of motor neurons. A number of ALS risk factors, including genetics, environmental exposures, and lifestyle habits, have been identified.
Amyotrophic lateral sclerosis (ALS) is characterized by progressive muscle weakness. Usually, the first symptoms include weakness in the hands or feet, causing problems with writing, gripping objects, or walking. In about one-third of patients, however, the first symptoms affect muscles around the mouth and throat, usually manifesting as issues speaking or swallowing.
Amyotrophic lateral sclerosis (ALS) most commonly manifests between the ages of 55 and 75, and the disease is more common in men than women. Other risk factors for ALS include a family history of the disease, smoking, excessive exercise, and exposures to toxins like pesticides.
In the early disease stages, people with amyotrophic lateral sclerosis (ALS) often struggle with activities that require fine hand motor skills, like writing or buttoning a shirt. As the disease progresses, muscle weakness becomes more severe and spreads throughout the body, with most patients eventually progressing to have little or no ability to move under their own power. People with ALS often experience difficulty eating and speaking, and breathing problems are common.
The average life expectancy for someone with amyotrophic lateral sclerosis (ALS) is about two to five years after the initial onset of symptoms. However, it is estimated that about 20% of ALS patients live more than five years after symptom onset, and about 10% will live past 10 years.
Related Articles

 Fact-checked by
Fact-checked by