Experimental gene therapy CTx1000 extends survival in mice
In lab studies, new treatment seen to stop ALS and FTD from progressing
Written by |
An experimental gene therapy called CTx1000, which is designed to reduce toxic buildups of the protein TDP-43 in nerve cells, was found to significantly extend survival and improve motor function in mouse models of amyotrophic lateral sclerosis (ALS) and the related disorder frontotemporal dementia, known as FTD.
According to the team of Australian researchers developing the treatment candidate, it “could be a game changer” for treating these two neurodegenerative diseases, as stated in a press release.
“In lab conditions, we saw CTx1000 stop [ALS] and FTD from progressing even at very advanced stages, and resolving the behavioural symptoms associated with FTD,” said Yazi D. Ke, PhD, a professor at Macquarie University, in Australia, and co-author of the study.
CTX1000 is now being developed by Celosia Therapeutics, a spin-out company formed by scientists at Macquarie. The experimental gene therapy is now in preclinical development, and researchers hope to start clinical testing in about two years.
“We have great hopes that when this progresses to human trials, it will not only stop people from dying from both [ALS] and FTD, but even allow patients to regain some of the lost function through rehabilitation,” Ke said.
A study detailing the laboratory findings, titled “Targeting 14-3-3[theta]-mediated TDP-43 pathology in amyotrophic lateral sclerosis and frontotemporal dementia mice,” was published in Neuron.
Experimental gene therapy targets protein ID’d as likely disease driver
Though the causes of ALS aren’t fully understood, abnormalities in the TDP-43 protein have been identified as a likely driver of the disease in about 97% of all ALS cases.
Nerve cells rely on TDP-43 to function, and normally this protein is located in the nucleus — the central cellular compartment that houses DNA. But in ALS, an abnormal version of the TDP-43 protein ends up misplaced outside the nucleus, where it forms clumps that are toxic to nerve cells. These clumps are observed in FTD, occurring in nearly 50% of patients.
In this study, the team of scientists performed a battery of cell experiments aiming to better understand exactly how TDP-43 moves out of the nucleus in these diseases. The team found that the abnormal versions of TDP-43 seen in ALS and FTD are able to stick to another protein called 14-3-3. The researchers noted that 14-3-3 is specifically the theta variant of this protein.
Importantly, the results indicated that this interaction is much stronger for the abnormal forms of TDP-43 that are associated with ALS and FTD. The normal version of TDP-43 found in nerve cells could also bind to the 14-3-3 protein, but much less strongly.
The scientists found that this interaction is key for moving TDP-43 out of the nucleus. When 14-3-3 levels were increased in cell or animal models, the amount of toxic TDP-43 outside the nucleus also rose.
In further experiments, the scientists zeroed in on the exact part of the 14-3-3 protein that binds abnormal TDP-43. They demonstrated that removing this particular part of the protein could prevent the interaction between TDP-43 and 14-3-3.
Analyses of brain samples from people with sporadic ALS showed increased 14-3-3 levels compared with brains from people without neurological disorders, consistent with the idea that this protein plays a role in driving the disease.
However, brains from people with familial ALS — another form of the disease that can be caused by mutations in the genes C9ORF72 or SOD1 — had normal 14-3-3 levels. That indicates that this mechanism may not apply in those genetic forms of ALS, the researchers said.
Treatment found effective in lab even at late stages of ALS
After defining this new disease mechanism, the researchers designed CTx1000 as a potential therapy to reduce toxic TDP-43.
The experimental gene therapy works by delivering into cells a gene that provides instructions for making the section of 14-3-3 that binds to toxic TDP-43. It attaches to a molecular sequence that cells normally use to signal proteins for destruction.
The basic idea is that the modified 14-3-3 protein binds to toxic TDP-43, and then both proteins are destroyed — thus allowing clearance of the toxic protein.
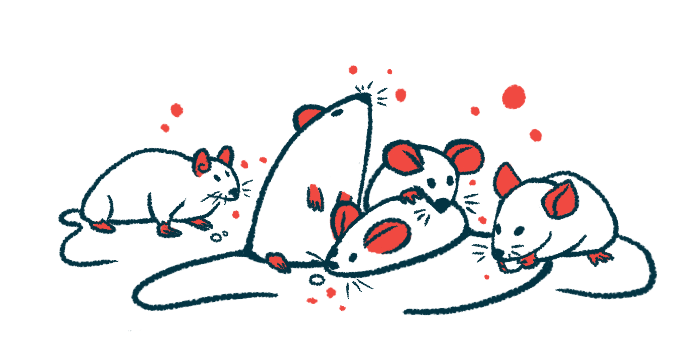
After creating the novel therapy, the researchers tested it in mouse models, and the results were generally positive: CTx1000 treatment reduced toxic TDP-43 buildups as designed, and treated mice showed less severe symptoms and tended to survive longer. Beneficial effects of treatment were seen when gene therapy was given at either early or advanced disease stages.
We have the potential for CTx1000 to be a one-shot treatment that can help people even at late stages of the disease. … [It] would quite literally be a light at the end of the tunnel that patients and their families just don’t have now.
“There is such a desperate need for new drugs for neurodegenerative diseases like [ALS], and this is an exciting new therapeutic with enormous potential,” said Brenton Hamdorf, MD, CEO of Celosia.
“We have the potential for CTx1000 to be a one-shot treatment that can help people even at late stages of the disease,” Hamdorf said, adding that the gene therapy “then … would quite literally be a light at the end of the tunnel that patients and their families just don’t have now.”
Annika van Hummel, PhD, another study co-author, said it was “particularly exciting” for the researchers to find that the therapy “was effective both before and after the onset of symptoms.”
“We wanted to prove beyond a doubt that this would work in different situations, and it resulted in clear improvements in both symptoms and brain pathology,” van Hummel said.
Altogether, the researchers concluded in the study that their work provides “proof-of-concept for a potential disease-modifying gene therapy.”
The team stressed, however, that additional preclinical work, such as safety tests, will be needed before the CTx1000 can be brought to clinical testing.