Familial ALS Mutation Seen to Turn Protein That Binds to RNA Toxic, Ultimately Killing Motor Neurons
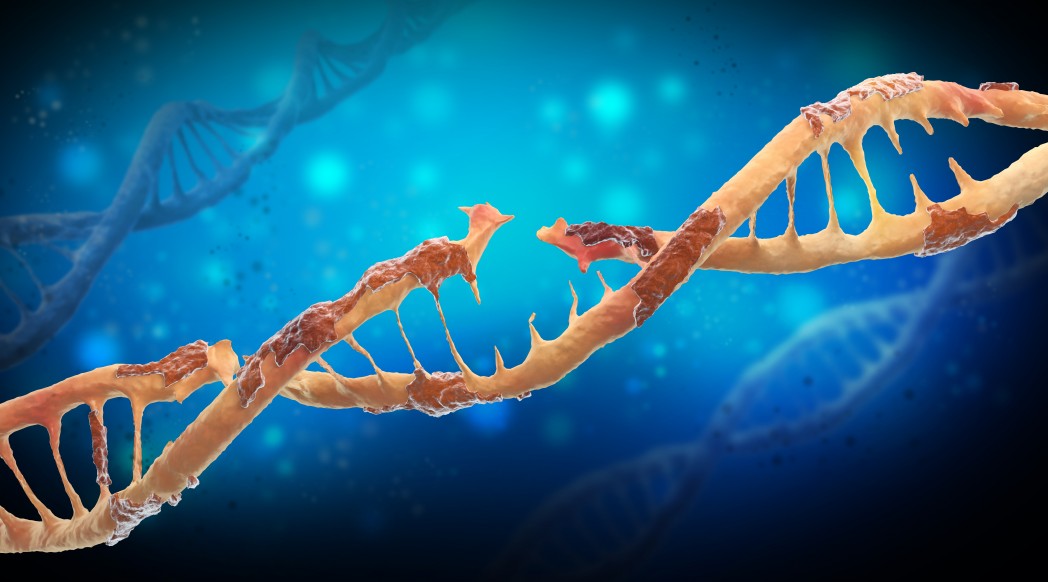
A mutation, causing an inherited type of amyotrophic lateral sclerosis (ALS), kills motor neurons by giving the protein it produces toxic properties. This protein, which normally binds to RNA, disrupts all RNA processing in the neurons to effectively take away their ability to survive.
The study, “Protein-RNA Networks Regulated by Normal and ALS-Associated Mutant HNRNPA2B1 in the Nervous System,” published in the journal Neuron, supports the development of treatments targeting RNA.
Researchers pointed out, however, that such treatments will only benefit patients with specific mutations in genes coding for RNA-binding proteins.
Surprisingly, many patients with familial forms of ALS (about 10 percent of all ALS cases) carry mutations in genes coding for proteins that bind RNA. Researchers at the University of California, San Diego School of Medicine homed in on a protein called hnRNP A2/B1.
“Our findings are a significant step forward in validating RNA-based therapy as a treatment for ALS,” Gene Yeo, PhD, a professor of cellular and molecular medicine at UCSD and the study’s senior author, said in a news release.
The research team was investigating how RNA-binding proteins control the production of certain proteins in ALS. They recruited four patients with familial ALS, and two healthy control individuals for the study. Participants only had to donate a bit of skin, as the rest of the experiments were done in a lab dish.
The approach uses a method called induced pluripotent stem cells, whereby skin cells are first turned into stem cells, which can then be pushed to develop into motor neurons. Three of the patients had mutations in hnRNP A2/B1, while the third patient carried another mutation.
This method allows scientists to study motor neurons having the same genetic makeup as a patient. To see what was going on, the team screened the activity of thousands of genes in the nerve cells.
They discovered that the mutation not only rendered hnRNP A2/B1 useless, it also made the mutant protein toxic for the cells. When mutant hnRNP A2/B1 was present in motor neuron cells, it disturbed all RNA processing in the cell, ultimately causing it to die.
As environmental factors likely contribute to the development of ALS in people who have an increased genetic risk, researchers also investigated the double impact of hnRNP A2/B1 and environmental stress.
They noted that in motor neurons from ALS patients, hnRNP A2/B1 ended up in a part of the cell called stress granules. This did not seem to happen in cells from healthy people.
“Drugs that lower the exaggerated reaction to stressors … may also prove a powerful therapeutic strategy,” Dr. Yeo said. “It is likely that multiple, multi-directional shots at goal will be needed to treat this debilitating disease.”