High Body Mass Index and Weight Gain with Aging Linked to Lower Risk of ALS in Norwegian Population Study
Written by |

People who have a high body mass index or gain weight as they age may be at a lower risk of amyotrophic lateral sclerosis (ALS), according to a large population study done in Norway.
Those who were obese or got heavier through time had a more than 30 percent lesser risk of developing ALS, compared to people with low-to-normal weight and those who maintained their figure or lost weight. The study’s researchers, however, stressed that genetics might be a factor in risk for this disease and did not recommend weight gain.
The study “High BMI is associated with low ALS risk – A population-based study” was published in the journal Neurology.
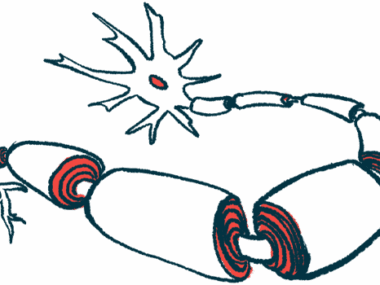
ALS, also known as Lou Gehrig’s disease, is a progressive neurological disease that destroys nerve cells in the brain and spinal cord, causing severe disability.
Recently, scientists have been exploring if weight and nutritional status could be possible prognostic factors of ALS. In their studies, they are trying to find evidence of whether and how these factors influence the disease’s risk or clinical course.
Body mass index (BMI) is a measure of a person’s body size and nutritional status. It is defined as a person’s weight in kilograms divided by the square of the person’s height in meters (kg/m2).
People are considered underweight if they have a BMI below 18.5 kg/m2, healthy if it is between 18.5 and 24.9, overweight (or pre-obese) if they have a BMI of 25 to 29.9, and obese with a BMI 30 or higher.
To investigate the relationship between BMI, weight change and ALS risk over time, researchers with the Institute of Clinical Medicine, University of Oslo, conducted a large population-based study.
They reviewed a Norwegian database that included BMI measurements for most citizens living in Norway between 1963 and 1975 — nearly 1.5 million people. They identified 2,968 ALS cases during a mean follow-up of 33 years (maximum 54) that concluded in 2017.
Information on lifestyle, health, and changes in weight over time was also collected for many study participants.
Researchers found that people with a higher BMI were associated with a lower risk of developing ALS, in both sexes and across ages typical for ALS onset.
For every 5-unit increase in BMI over time in people in the low-normal weight range, there was a 17% lower risk of developing ALS later on.
Among the 468,853 people in that low-normal range, 1,002 developed ALS — corresponding to 0.21% — whereas among the 139,158 people in the obese range, 182 people (0.13%) developed ALS.
At the 50-year mark, participants had a 31% lower risk of developing ALS for every 5-unit increase in BMI.
Those who were obese or overweight at the study’s start had a 34% and 18% lower chance, respectively, of disease onset compared to those in the low-normal BMI range.
Moreover, the team noted that people who gained the most weight over time had a 37% lower risk of ALS than did those who maintained or lost weight.
The relationship between high BMI and lower ALS risk remained after adjusting for smoking, cholesterol levels, and physical activity.
“High BMI and weight gain are associated with low ALS risk several decades later. The strength of the association between BMI and ALS risk increases up to 50 years after BMI measurement,” the researchers wrote.
But the study’s leader, Ola Nakken, MD, of the University of Oslo, stressed that the relationship drawn could be influenced by factors outside the study’s scope, like genetics, and gaining weight should not be seen as way of preventing ALS.
“It is important to note that while our study found a link between high BMI and a lower risk of ALS, it is possible that genetics could make a person more likely to have both a low BMI and a higher risk of ALS without one causing another,” Nakken said in a press release.
“People must not interpret the results of our study as a suggestion that gaining weight may prevent ALS. Plus, the health risks of having a high BMI would be greater than any protective effect.”
Still, most ALS cases “do not appear to have a genetic cause, and an increasing body of evidence suggests that there may be a link between a fast metabolism that can lead to a low BMI and ALS,” Nakken added. “Much more research is needed to further examine the relationship between BMI and ALS.”
One limitation of this study, the researchers said, was that most participants were white, so its results may not hold for other populations.