Specific Nerve and Other Cells in Spine Unique to ALS Patients and May Be Early Markers of Disease, Study Says
Written by |
Specific populations of neurons and associated cells in the spinal cord of people with sporadic amyotrophic lateral sclerosis (ALS) may serve as early biomarkers for the disease, a study has found.
The newly discovered populations offer scientists a chance to learn more about the first steps underlying ALS and potentially identify new targets for treatments.
The study, “Predicting disease specific spinal motor neurons and glia in sporadic ALS,” was published in the journal Neurobiology of Disease.
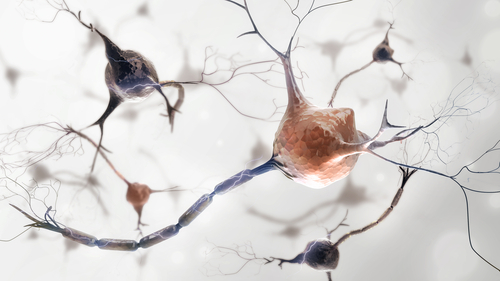
ALS, a progressive neurological disease, is marked by a gradual death of motor neurons, the nerve cells responsible for controlling voluntary muscle movement. With their loss, the brain and spinal cord are no longer able to control muscle movement, and muscles waste (atrophy) and weaken.
ALS has what is known as a “focal onset” when muscle weakness and paralysis start with an arm or a leg, with nerve cells along specific regions of the spine affected. As the disease progresses, weakness spreads and motor neurons in both the spinal cord and brain die.
Early diagnosis has been hampered by the lack of biomarkers that hint at the disease’s initial stages. But some scientists believe changes within the spinal cord may occur before patients notice their first symptoms, changes that could be tracked and serve as early biomarkers.
Join our ALS forums: an online community especially for patients with Amyotrophic Lateral Sclerosis.
Scientists already know that neuroinflammation plays a role in sporadic ALS (of unknown cause), the disease’s most common form. Activated glia (non-neuronal cells of the nervous system) and infiltrated immune cells are involved in this process, but how these cells interact and lead to motor neuron death is less clear.
Researchers at the University of Illinois at Chicago (UIC) wanted to delve deeper into this relationship and its implications for sporadic ALS.
They used new computational tools to look again at genetic data captured from spinal motor neurons of patients who died from focal-onset ALS, and who consented to have their nerve tissue collected after death.
In specific, they wanted to disentangle the different cell types present at sites within the spinal cord from those at nearby sites most affected by the disease.
“Since there must be cellular changes occurring in spinal cord regions adjacent to areas where the disease has clearly affected motor neurons in the spine, we wanted to look at neurons from these adjacent areas to determine if they are different from healthy tissue,” the study’s senior leader, Fei Song, a professor at the UIC College of Medicine, said in a press release.
Interestingly, they found two populations of spinal motor neurons at less affected regions that were unique to sporadic ALS patients, compared to patients without neurological disorders (control samples).
One type inversely correlated with patient survival, meaning a higher presence led to poorer survival.
Scientists also found that spinal neurons of ALS patients had greater numbers of two unique groups of immune cells, called microglia and infiltrated macrophages, that were absent in control samples. Further tests suggested these immune cells were activated.
Microglia is both a glia and an immune cell that normally works to protect our central nervous system (CNS; the brain and spinal cord) from injury and disease. Macrophages typically reside in multiple tissues throughout the body, with some infiltrating the CNS. Depending on the context, both cells can be neuroprotective and anti-inflammatory. But they can also promote neuroinflammation, as in the case in ALS.
“Our findings support the hypothesis that neuro-glia physical interactions are important in pathogenesis [disease development], and targeting disease-specific motor neurons and/or glia could be a useful therapy to slow disease progression,” the researchers wrote.
ALS has “no effective treatment to stop the disease progression … So, new drug targets, especially ones that could be given in the earlier stages of the disease, are very much needed,” Song said.
“We found a novel and unique subtype of motor neurons in these patients never before reported,” Song added. “Now that we have identified new subtypes of motor neurons and microglia present in ALS patients, we can begin to further study their roles in contributing to disease progression.”