New Spinal Delivery Method Renders Stem Cell Therapy Safer, More Effective for ALS, Other Diseases, Early Study Suggests
A new spinal cell delivery method may reduce the risks and boost the effectiveness of stem cell therapy designed to regenerate the nervous system in neurodegenerative diseases such as amyotrophic lateral sclerosis (ALS), an early study in rats has found.
The study, “Spinal parenchymal occupation by neural stem cells after subpial delivery in adult immunodeficient rats,” was published in the journal Stem Cells Translational Medicine.
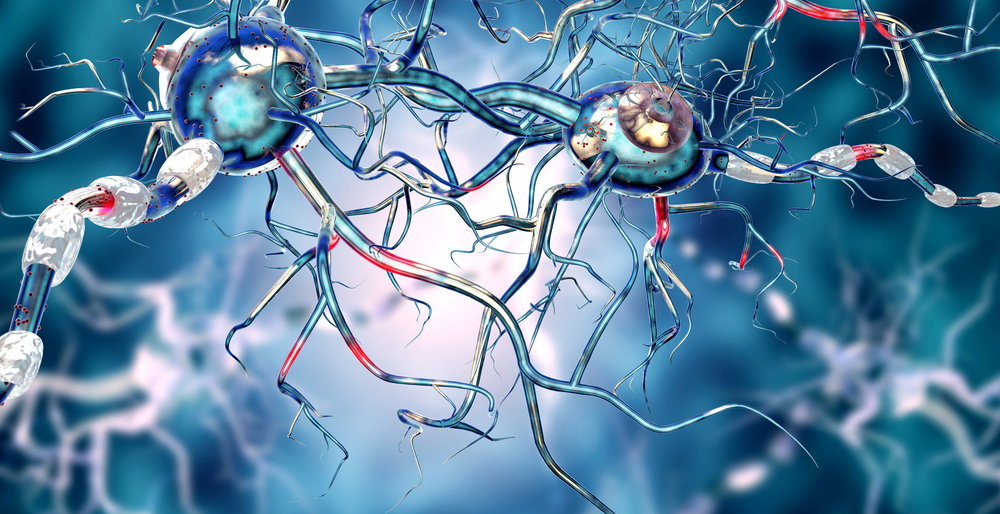
Neural precursor cells (NSCs) — stem or progenitor cells with the ability to generate several types of spinal cord and brain cells — hold great potential to repair spinal cord injuries and regenerate nervous tissues in people with neurological diseases, including amyotrophic lateral sclerosis (ALS).
Stem cell transplants or cell-replacement therapy using NSCs has been emerging as a potential new approach to treating ALS, aiming to regenerate damaged or dying neurons and other important cells that support them.
Current spinal cell delivery techniques, however, are invasive and risky, involving direct injections into the spinal parenchyma, where neurons and nerve fibers run through the spinal column into the brain.
“As such, there is an inherent risk of (further) spinal tissue injury or intraparechymal bleeding,” Martin Marsala, MD, professor at University of California San Diego School of Medicine, said in a press release. In addition, this type of injection limits delivery in many spinal segments.
Now, a team led by physician-scientists at the university have developed a new method for delivering NSCs which is potentially safer and more effective.
The new technique involves injecting cells into the spinal subpial space — a space between the pial membrane, the innermost layer surrounding the brain and spinal cord, and the superficial layers of the spinal cord. This means the injection does not touch the nervous tissues of the spinal cord which makes it less invasive and potentially safer.
Using this technique to inject human NSCs in rats, the team observed a potent and widespread propagation of injected cells throughout the spinal cord and to the brainstem (the base of the brain that is connected to the spinal cord).
Six to eight months after, the rats’ spinal cords were nearly fully occupied by human cells, which had converted into glial-like cells. More specifically, these cells acquired features of oligodendrocytes and astrocytes.
Neuroglia, or glial cells, are a large and important group essential for the well-being of neurons, providing them with support and protection. They can influence neuronal activity in the brain and spinal cord. In fact, neuroglia exceed the number of neurons by at least 10 to one.
“This injection technique allows the delivery of high cell numbers from a single injection,” said Marsala.
“Cells with proliferative properties, such as glial progenitors, then migrate into the spinal parenchyma and populate over time in multiple spinal segments as well as the brain stem. Injected cells acquire the functional properties consistent with surrounding host cells,” he said.
Of note, all animals kept a normal neurological function after receiving the injections. This is the first study to demonstrate a successful spinal cell repopulation by neural stem cells, without using an invasive approach.
The researchers said the findings show that subpial delivery “is highly effective” for repopulating the whole spinal cord with stem cells, and “has a potential for clinical use in cell replacement therapies for the treatment of ALS, multiple sclerosis, or spinal cord injury.”
The method will likely accelerate and improve the potency of treatments where broad regeneration of glial cells, including oligodendrocytes or astrocytes, is desired, the team said.
While the root cause of ALS is damage and death of motor neurons — the neurons responsible for voluntary muscles — evidence points to the important roles played by glial cells in this neurodegenerative process.
Another important point is that ALS leads to widespread neuronal damage, affecting motor neurons throughout the spinal cord and in the brainstem. Thus, a more homogeneous distribution of NSCs along the spinal cord could increase the neuroprotective and regenerative effect of these cells.
Other observations support the benefits of this new delivery system for treating ALS. Upon subpial delivery, stem cells repopulated a type of glial cell population living in the spinal cord’s outermost layer and that was able to produce the enzyme superoxide dismutase (SOD).
Abnormalities in SOD have been associated with familial and sporadic cases of ALS. The gene encoding the enzyme, SOD1, is one of the most commonly mutated in people with familial ALS.
In the researchers’ opinion, the new spinal delivery approach may offer additional therapeutic effects by restoring the protective roles of glia at least in ALS caused by SOD1 mutations.