C9ORF72 Mutations Disrupt Cellular RNA and Protein Processing, Study Finds
Mutations in the C9ORF72 gene, the most common cause of amyotrophic lateral sclerosis (ALS), lead to changes in how cells process ribonucleic acid (RNA) and protein, a new study shows, shedding light on the mechanisms through which such mutations cause disease.
Notably, researchers have identified a protein involved in this defective processing, which may be a useful therapeutic target for ALS.
The study, “Nucleocytoplasmic Proteomic Analysis Uncovers eRF1 and Nonsense-Mediated Decay as Modifiers of ALS/FTD C9orf72 Toxicity,” was published in Neuron.
Mutations in C9ORF72 account for up to 40% of familial ALS cases and 7% of sporadic cases, yet the precise mechanisms through which these mutations cause disease are still a subject of investigation. Previous research has suggested that mutant C9ORF27 leads to changes in how proteins are distributed throughout the cell.
“What we wanted to identify, however, was what are the proteins that are redistributed as a result of this trafficking defect,” Evangelos Kiskinis, PhD, an assistant professor at Northwestern University and senior author of the new study, said in a press release.
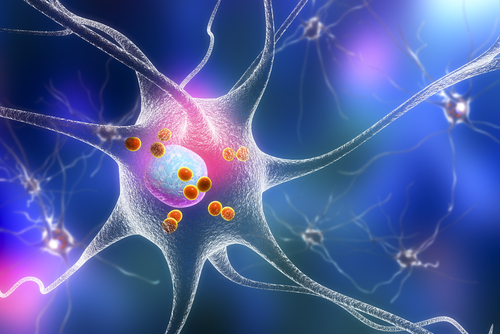
To do this, the researchers used subcellular fractionation — basically, they separated the nucleus (the cellular component that houses DNA) from the rest of the cell (the cytoplasm). Then, using mass spectrometry, they analyzed the proteins that were present in each of these cellular compartments, in cells with or without mutant C9ORF72.
This identified 126 proteins that were distributed differently in cells with the mutation. Many of these proteins play important roles in cellular processes, particularly RNA and protein metabolism.
In particular, the researchers focused on a protein called eRF1, whose depletion caused most of the protein toxicity in fly models carrying mutant C9ORF72.
Typically, this protein has two main jobs that are interrelated: when proteins are made (translated) from RNA, there is a signal in the RNA molecule that indicates where protein production should stop. In normal translation, eRF1 binds this signal, helping to release the newly-formed protein from the cell’s protein-making machinery. But, if the RNA molecule in question has certain abnormal or disease-like features, eRF1 can target the RNA for destruction through a process called nonsense-mediated decay (NMD).
Normally, eRF1 is located in the cytoplasm. But in cells harboring mutant C9ORF72, the protein shifted its location to invaginations (folds) in the membrane that surrounds the nucleus, called the nuclear envelope, where it triggers widespread NMD. This shift in location was found in multiple models of ALS, including patient-derived motor neurons and fruit fly models.
“What we found was that this protein accumulates within nuclear invaginations, and triggers a reduction in protein translation and an increase in the degradation of RNA molecules including the mutant C9orf72 transcript itself,” Kiskinis said.
This suggests “a model where NMD safeguards neurons from toxic RNA molecules,” the researchers wrote. Essentially, the rationale is that eRF1 activates NMD to remove mutant C9ORF72 RNA molecules before they can cause further damage (i.e. before they are translated into toxic protein products).
“This study is exciting because, based on an unbiased approach, our findings pointed to a specific RNA degradation pathway, which may be a key underlying component of disease,” said Elizabeth Daley, a graduate student at Northwestern and co-author of the study.
Beyond the basic scientific understanding of how a mutation leads to cell stress, “the NMD pathway and its regulatory elements may represent a therapeutic approach that could be broadly relevant for ALS,” the researchers wrote.
“The potential therapeutic relevance of this model could be explored either through small molecules that would activate NMD or directly through gene therapy approaches,” they said.
Interestingly, the researchers also carried out protein-localization experiments with cells harboring mutations that are associated with other neurodegenerative diseases, namely Huntington’s disease and spinocerebellar ataxia type 1.
Like C9ORF72, these mutations led to significant changes in protein distribution within the cells, but there was relatively little (less than 5%) overlap in the specific proteins that were affected by each of the three mutations assessed.
“These results suggest that impaired [protein trafficking between the nucleus and cytoplasm] could be broadly implicated in other neurodegenerative diseases,” the researchers wrote.
Further studies may uncover the reasons for specific differences in the proteins affected, and could be useful in advancing understanding of these diseases or finding new treatment strategies for them.