Masitinib Helps Keep Inflammatory Mast Cells From Spinal Cord
Mast cells, a type of immune cell, infiltrate the spinal cord of amyotrophic lateral sclerosis (ALS) patients and rodent models of the disease, exhibiting pro-inflammatory features that are likely involved in motor neuron and microvasculature damage, a study suggests.
Notably, treating these mice models with masitinib — an experimental oral therapy by AB Science that showed promise as an add-on treatment in a clinical trial in ALS patients — lowered the number of mast cells in the spinal cord and lessened microvascular abnormalities.
These findings support evidence of mast cells’ damaging role in ALS, and show “for the first time that mast cell number and trafficking into the spinal cord of an ALS animal model were downregulated by masitinib, with subsequent neuroprotective effects in ALS,” Emiliano Trías, PhD, the study’s senior author at the Institut Pasteur de Montevideo, in Uruguay, said in a press release.
“These data further reinforce the rationale for masitinib’s potential neuroprotective effect in ALS patients,” Trías added.
The study, “The pathogenic role of c-Kit+ mast cells in the spinal motor neuron-vascular niche in ALS,” was published in the journal Acta Neuropathologica Communications.
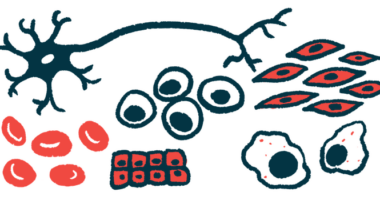
Mast cells are a type of immune cell that, upon activation, undergo a process called degranulation that boosts inflammation and blood vessel permeability.
Excessive mast cell accumulation and activation have been associated with chronic neuroinflammation and disruption of the blood-brain barrier and brain-spinal cord barrier. These barriers are highly selective membranes that prevent microbes and potentially harmful molecules and cells in circulation from entering the central nervous system (CNS; the brain and spinal cord).
Previous studies showed that mast cells contribute to ALS through close contact with degenerating motor neuron fibers and neuromuscular junctions — both located outside the CNS. The neuromuscular junction is the site of contact between a nerve cell and a muscle cell.
While mast cells have been reported in the CNS of ALS patients, how these cells enter the central nervous system and how they interact with motor neurons and microvasculature (small blood vessels) in the spinal cord remains unclear.
Trías and his team, along with colleagues in the U.S. and France, analyzed the presence, features, and dynamics of mast cells in the spinal cord of five deceased ALS patients and of rodent disease models.
They found that mast cells and their precursors infiltrate and accumulate in the degenerating spinal cord of both ALS patients and the rodents, and show degranulating features, suggesting their activation. Similar features were not observed in the spinal cords of healthy individuals and rodents.
Mast cells in ALS patients and models were mainly found between motor neurons and nearby small blood vessels of the blood-spinal cord barrier (BSCB), which exhibited marked abnormalities that allowed mast cell precursors to reach the spinal cord.
Further analysis in the rodent models showed that mast cell precursors, positive for a cell surface receptor protein called c-Kit, accumulated near motor neurons and astrocytes (neuron-supporting cells) producing stem cell factor (SCF), a protein that binds to c-Kit, activating it.
Mast cell precursor infiltration and subsequent maturation in the spinal cord “seem to be a complex process controlled by the integrity of BSCB and the [overproduction] of SCF in reactive astrocytes and neurons,” the researchers wrote.
In addition, mast cells can “damage the BSCB suggesting a bidirectional pathogenic [disease-associated] process that could be relevant for the integrity of the motor neuron-vascular niche,” the team added.
Given that masitinib — which has shown anti-inflammatory and neuroprotective effects in ALS — is a suppressor of c-Kit, the researchers then evaluated an ALS mouse model given with the experimental therapy.
Masitinib treatment was found to significantly reduce both the number of infiltrating mast cells (by 50%) and microvascular abnormalities (by 30–40%) in the animals’ spinal cord.
These results “are consistent with a masitinib protective effect via c-Kit inhibition, preventing the trafficking of mast cell precursors and mast cell local [maturation] in the motor neuron-vascular niche,” the researchers wrote.
They also highlight “a previously unknown pathogenic [disease-associated] mechanism triggered by [mast cells] in the ALS motor neuron-vascular niche that might be targeted pharmacologically,” the team added.
Findings add to the growing body of studies highlighting the beneficial effects of masitinib in ALS, including a survival benefit when administered at an early stage of the disease.
Luis Barbeito, MD, PhD, a study author and head of the neurodegeneration laboratory at Institut Pasteur in Montevideo, said: “these new data further corroborate the biological plausibility for using masitinib in ALS and support previous clinical findings that masitinib may provide a greater benefit if administered at an early stage of the disease course.”
Masitinib’s therapeutic effects are being confirmed in a Phase 3 clinical trial, called AB19001 (NCT03127267), in up to 495 adults with early stage ALS. Those enrolled are being randomized to oral masitinib or to a placebo, both given twice daily as an add-on to riluzole for 48 weeks.
One of the study’s 12 scientists is a co-founder and shareholder of AB Science.