2 proteins identified as potential therapeutic targets in FUS-ALS
Suppressing these proteins in worm model found to lessen ALS hallmarks
Written by |

Targeting two particular proteins, called H1.2 and PARP1, may lessen the severity of amyotrophic lateral sclerosis (ALS) linked to mutations in the FUS gene, a study shows.
Researchers found that a severe FUS mutation increased the interaction of the resulting FUS protein with both H1.2 and PARP1, which is involved in a process of protein modification called poly ADP-ribosylation (PARylation). This enhanced interaction promoted several ALS hallmarks, including the formation of toxic FUS clumps and neurodegeneration.
On the other hand, suppressing either H1.2- or PARP1-like proteins in a worm model carrying that severe FUS mutation lessened several of these hallmarks.
“Considering all our data, our findings indicate a link between PARylation, H1.2 and FUS with potential therapeutic implications,” Hafiza Alirzayeva, PhD, the study’s first author at the University of Cologne, in Germany, said in a university press release.
The study, “ALS-FUS mutations cause abnormal PARylation and histone H1.2 interaction, leading to pathological changes,” was published in the journal Cell Reports.
FUS mutations implicated in familial and sporadic cases of ALS
ALS is marked by the progressive degeneration and death of motor neurons, the nerve cells that control voluntary movement. Mutations in the FUS gene, which encodes the FUS protein, cause about 5% of familial ALS cases and about 1% of sporadic ALS cases, and are associated with early-onset forms.
The FUS protein is typically found in the cell nucleus (which contains all genetic information), but FUS mutations cause it to move outside the nucleus and form toxic clumps in motor neurons, eventually promoting their death.
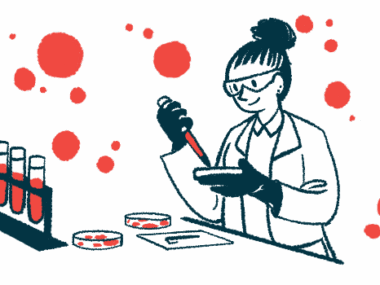
To better understand the molecular effects of ALS-causing FUS mutations, the researchers analyzed FUS protein interactions in lab-grown human motor neurons carrying P525L, the most aggressive FUS mutation, and neurons without the mutation.
Motor neurons were derived from induced pluripotent stem cells (iPSCs), which are lab-made stem cells generated from mature cells that are able to grow into almost any type of cell, including motor neurons.
Results showed that carrying the P525L mutation changed the interactions between the FUS protein and other proteins and enzymes within motor neurons, with some interactions being lost and others being gained or increased.
Histone H1.2 showed strongest interaction with mutated FUS protein
Histone H1.2, a protein involved in wrapping DNA inside cells, showed the strongest interaction with the mutated FUS protein, and stronger than observed with the healthy FUS protein. Notably, this increase in FUS-H1.2 interaction was also seen in patient-derived iPSCs with other FUS mutations.
The PARP1 enzyme also showed a stronger interaction with mutated FUS relative to nonmutated FUS. PARP1 promotes PARylation, a process involving the addition of certain chemical tags to proteins.
When the researchers suppressed H1.2 production in P525L-mutated motor neurons, this was sufficient to reduce FUS aggregation, without affecting total FUS protein levels. This was associated with more mutated FUS protein in the nucleus, its natural location.
Moreover, lowering H1.2 levels was linked to reduced death of motor neurons producing either the mutated or normal FUS protein. In turn, increasing H1.2 levels beyond the norm boosted cell death, and to a greater extent in cells with mutated FUS.
This suggests that a greater FUS-H1.2 interaction promotes FUS mislocalization outside the nucleus, resulting in toxic aggregation and neurodegeneration, the team noted.
Further experiments showed PARP1 was required for FUS-H1.2 interaction and that all three proteins interacted, and to a greater extent with the mutated FUS protein.
“These results indicate that PARP1, H1.2, and FUS may form a complex whose assembly is [boosted] by mutant FUS,” the team wrote.
In addition, PARylation was increased in motor neurons producing mutated FUS, and suppressing this protein modification process reduced the cells’ death.
Findings tested in worm model
The researchers then tested their findings in Caenorhabditis elegans, a tiny worm commonly used in research, that was genetically modified to produce the P525L mutated FUS protein across the nervous system. They specifically assessed the impact of reducing levels of the worm equivalent proteins to human H1.2 and PARP1.
Suppressing either H1.2- or PARP1-like proteins reduced mutated FUS clumping and lessened motor deficits. When the team promoted an overproduction of human H1.2, they saw a faster aggregation of mutant FUS protein and worse motor problems.
“Altogether, our data indicate that H1.2 and PARP1 could be potential therapeutic targets to decrease FUS-related aggregation and neurodegeneration,” the researchers wrote.
While this study focused on an FUS mutation, clumps of nonmutated FUS are also found in sporadic ALS cases, suggesting that these findings may have implications for all ALS cases.
The researchers now plan to investigate the role of these proteins in forms of ALS caused by mutations in other genes, as well as in sporadic ALS cases.
“We hope to show in further studies that our findings could have a potential impact on sporadic ALS as well, since that is the form that affects the overwhelming majority of patients,” said David Vilchez, PhD, the study’s senior author at the University of Cologne.