Tiny Brain Blood Vessels Stimulate Movement Nerve Cell Growth, Study Reports
The brain’s smallest blood vessels stimulate the growth of spinal cord nerve cells at an early stage of their development, researchers at Southern California’s Cedars-Sinai group report.
Their discovery, made with a tiny biological chip, could help shed light on the causes of amyotrophic lateral sclerosis (ALS).
The article they wrote about their research was titled “Human iPSC-Derived Endothelial Cells and Microengineered Organ-Chip Enhance Neuronal Development.” It appeared in Stem Cell Reports.
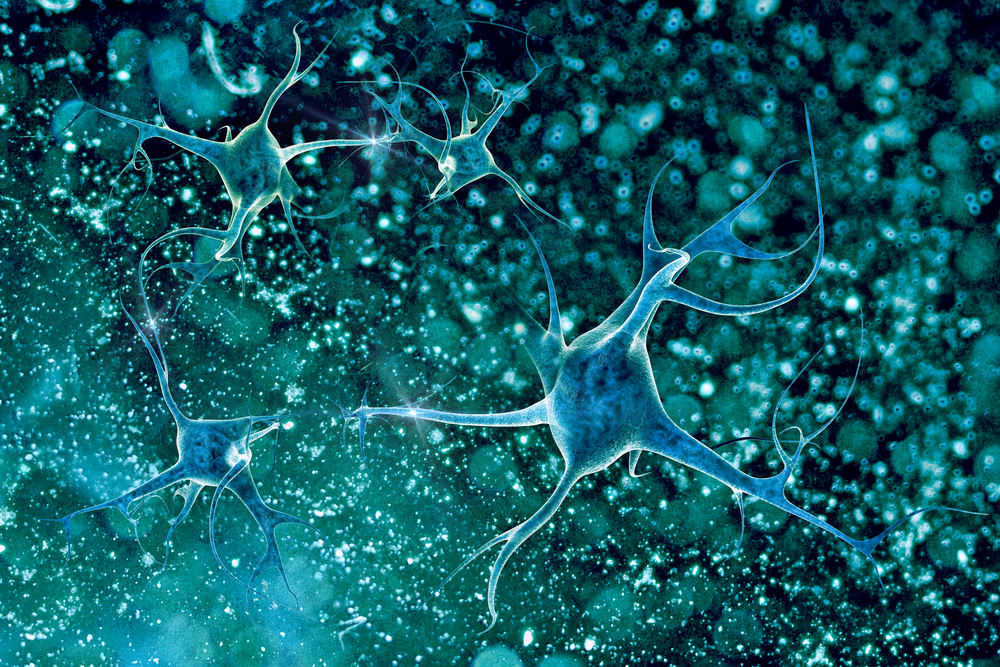
Tiny blood vessels that distribute oxygen, carbon dioxide and nutrients throughout the body are linked together closely in the brain to protect it against harmful invaders.
The cells in these capillaries help form the protective blood-brain barrier that interacts with developing nerve cells, including spinal motor neurons. These are nerve cells responsible for muscle movement.
Scientists also know that capillary cells share common molecular pathways with neurons early in the neurons’ development. But their influence on neuron maturation has been unclear.
The team decided to investigate their hypothesis that capillaries in the brain interact with spinal cord neurons to help the neurons mature.
They used a device about the size of a computer memory stick to replicate the shape and function of capillary cells and spinal motor neurons.
To do so, they collected skin cells from adults, then genetically reprogrammed them to create tiny brain blood vessel cells and spinal motor neurons. The see-through chip contained hollow channels, which researchers lined them with the cells. This gave them a window into the cells’ inner workings.
The brain capillaries interacted with the spinal cord neural tissue, making it possible for neurons to grow in an early stage of brain development, the researchers discovered.
“Until now, people thought these blood vessels just delivered nutrients and oxygen, removed waste and adjusted blood flow. We showed that beyond plumbing, they are genetically communicating with the neurons,” Dr. Samuel Sances, a postdoctoral fellow at the Cedars-Sinai Board of Governors Regenerative Medicine Institute, and first author of the study, said in a news release.
In an embryo, genes are turned on and off to direct early development. The research team’s work demonstrated that the brain’s smallest blood vessels not only turn on such genes but also help spinal motor neurons mature.
The results could help shed light on cell-cell communication behavior in certain neurodegenerative diseases, including ALS, and what role the interactions play in the onset of a disorder.
“This study told us something important about how our neurons develop,” said Dr. Clive Svendsen, a professor of Medicine and Biomedical Sciences who is director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute. He was senior author of the study.
Researchers plan to use the microdevice technology to study capillary and nerve cell communication in ALS patients and compare it to the interactions in healthy individuals.
This work is a result of a new Patient-on-a-Chip program that is a collaboration between Cedars-Sinai and Emulate in Boston. It pairs Cedars-Sinai’s innovative stem cell science with Emulate technology that creates true-to-life biology outside the body.
By placing a patient’s cells in a chip and exposing them to a drug, doctors may be able to learn more about how the patient is likely to respond to treatment.