Astrocytes in Nervous System Seen to Protect Motor Neurons from Toxicity of Clumps
Written by |
Astrocytes — cells of the nervous system cell that provide support to neurons — were seen to help protect motor neurons from damage caused by toxic protein clumps in a cell model of amyotrophic lateral sclerosis (ALS).
The study reporting this finding, “Distinct responses of neurons and astrocytes to TDP-43 proteinopathy in amyotrophic lateral sclerosis,” was published in Brain.
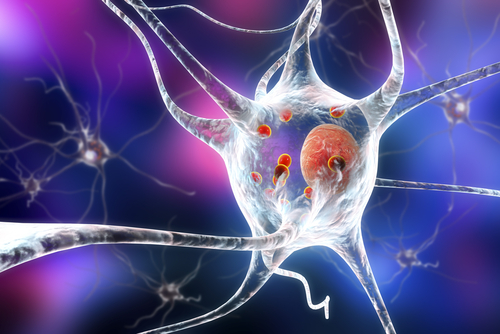
Astrocytes are cells in the nervous system with many important roles that support neurons, the cells that transport electric signals. In ALS, neurons — specifically motor neurons, which tell muscles when to move — die off. As such, neurons have been the focus of much cellular research in ALS, but far less is known about the role of astrocytes in the disease.
A molecular feature of ALS is the buildup of an improperly folded protein, TDP-43, that accumulates in the brain and contributes to motor neuron death. This protein is thought to act like a prion — that is, having some misfolded TDP-43 prompts other, seemingly normal TDP-43 molecules, to also fold inadequately and form clumps, a process called seeded aggregation.
The researchers created human motor neurons and astrocytes using induced pluripotent stem cells (iPSCs). Essentially, they collected skin cells from volunteers and reverse-engineered these cells into stem cells, a type of cell that is able to differentiate into other cell types.
These stem cells were prompted, using specialized biochemical signals, to differentiate into motor neurons or astrocytes.
Researchers then ‘seeded’ these iPSC-derived neurons and astrocytes by exposing them, in a lab culture, to tissue from the nervous system of a person who had died of sporadic ALS.
“It is thanks to the selfless donations from people with motor neuron disease, that we were able to study the interplay between motor neurons and astrocytes in conditions that closely resemble what happens in humans,” Katie Sidle, MRCP, a neurologist at University College London Hospitals and a study co-author, said in a press release. “These human cell models are a powerful tool for further studies of motor neuron disease and in the hunt for effective therapies.”
In motor neurons, misfolded TDP-43 was found to spread relatively rapidly: it affected 2% of cells after three days of exposure and 6.7% of cells after two weeks. Chemical treatment affecting the cells’ protein-recycling machinery (the proteasome) increased this spread; its use had the misfolded protein affecting 15% of cells after three days.
However, misfolded TDP-43 spread less in astrocytes, affecting around 5.8% of cells after chemical treatment. Motor neurons also died when TDP-43 concentrations were at their highest, while no cell death was observed for astrocytes.
Additional experiments with purified TDP-43 suggested that this protein is more toxic to motor neurons than to astrocytes.
“The resilience of astrocytes to both TDP-43 oligomer treatment and seeded aggregation observed here is intriguing and may be due to lack of cellular uptake of the oligomers, more efficient protein clearance machinery in astrocytes and potential neuronal receptor dependent mechanisms of toxicity,” the researchers wrote.
Researchers also tested whether TDP-43 could spread from motor neurons to astrocytes, or vice versa, by exposing one of these cell types to the other after it had been exposed to TDP-43. In both sets of exposure, the number of TDP-43-positive cells initially rose and then dropped, suggesting that the cells were able to clear some of the toxic protein.
“Cumulatively, these data from iterative co-culture paradigms raise the possibility that astrocytes may, at least initially, exhibit neuroprotective properties in the context of seeded TDP-43 proteinopathy,” the researchers wrote.
To further test this idea, they cultured motor neurons that had been exposed to TDP-43 clumps with astrocytes. This mixed culture significantly reduced the number of TDP-43-positive motor neurons, from 37.8% to 23.4%. And the number of motor neurons positive for caspase 3, a marker of cell death, dropped from 32.2% to 19.2%.
Similar results were also observed when motor neurons were grown in cell media that had previously contained astrocytes, suggesting this effect might be due to chemical signaling between the cells.
“It’s exciting that we’ve now found that [astrocytes] may play an important protective role in the early-stages of [ALS],” said Phillip Smethurst, PhD, a former postdoc at The Francis Crick Institute and a study co-author. “This has huge therapeutic potential — finding ways to harness the protective properties of astrocytes could pave the way to new treatments.
“This could prolong their rescue function or find a way to mimic their behaviour in motor neurons so that they can protect themselves from the toxic protein,” Smethurst added.





