Lymphoma Drug, AMD3100, Shows Promise in a Mouse Model of ALS
Written by |
A recent study in mice could provide the first step toward a new way of treating amylotrophic lateral sclerosis (ALS). The research report, “Chronic administration of AMD3100 increases survival and alleviates pathology in SOD1G93A mice model of ALS,“ was published on May 26 in the Journal of Neuroinflammation.
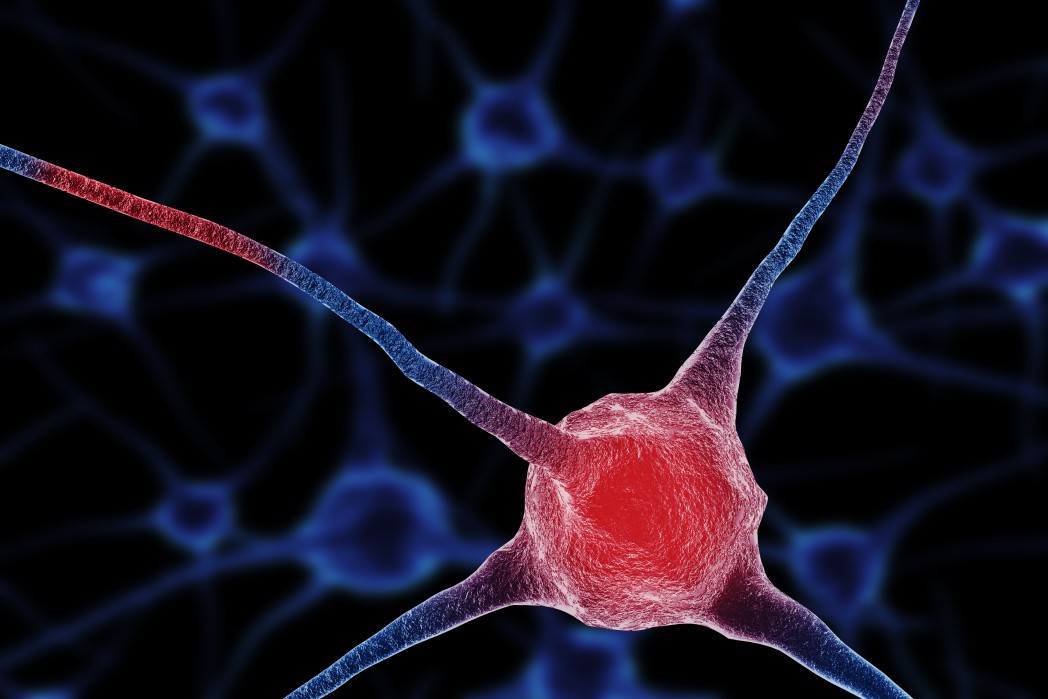
In ALS, nerve cells that control movement progressively die in the brain and spinal cord. Only one drug, riluzole, has been approved by the U.S. Food and Drug Administration (FDA) to treat ALS, but it is considered to have only modest effects on disease progression.
AMD3100, also called Mozobil and plerixafor, is an FDA-approved medication that may be promising for the treatment of ALS. It is already used as an immune system suppressant for stem cell transplant preparation to treat non-Hodgkin lymphoma or multiple myeloma. The drug may prevent the injury of nervous system cells by blocking a molecule known as CXCR4, which is part of an ALS cell-death cascade.
Inna Rabinovich-Nikintin of the Department of Molecular Microbiology and Biotechnology, George S. Wise Faculty of Life Sciences, Tel Aviv University in Israel, led the study, with Beka Solomon as the principal author. The scientists studied a mouse that had been genetically modified to have symptoms of ALS, known as the SOD1G93A mouse. They treated the animals with AMD3100 and tested their ability to move using a standard assessment of movement called the Rotatod test, which assesses strength and coordination.
Giving AMD3100 to the mice improved several of their ALS-like symptoms. It increased their lifespan, improved their ability to move, and prevented weight loss. AMD3100 also decreased the presence of microglia, cells that may contribute to inflammation — a heightened immune response that can contribute to the neuronal death the characterizes ALS. Inflammation is commonly seen in human patients with the disease. AMD3100 also decreased molecules made by microglia that contribute to inflammation, called cytokines.
Overall, the researchers concluded that “[t]he data presented here, relevant to the corresponding disease mechanism in humans, implicates AMD3100 as a possible candidate for ALS therapy with a multifaceted effect. As soon as a full understanding of its effects is reached, treatment based on this agent can move forward relatively fast in the pipeline, as AMD3100 was found safe and approved by the FDA for other indications.”
As noted, because AMD3100 is already FDA approved for other indications, it may be possible to quickly advance this medication through human clinical trials. A better understanding of how AMD3100 works in humans is needed, although this study may prove to be an important first step.