Changes in Aggregation of ALS-related Protein Revealed in Study
Researchers have detailed the structural changes that occur in the protein hnRNPA2 when it is mutated in diseases related to amyotrophic lateral sclerosis (ALS).
The study, “Mechanistic View of hnRNPA2 Low-Complexity Domain Structure, Interactions, and Phase Separation Altered by Mutation and Arginine Methylation” was published in the journal Molecular Cell.
A growing number of proteins have been identified as driving the formation of aggregates inside cells in individuals with degenerative diseases like ALS, multi-system proteinopathy, frontotemporal dementia and inclusion body myopathy.
Researchers already knew that in people with these conditions, proteins carry certain mutations that trigger their ability to generate aggregates inside cells and contribute to pathology.
Researchers wanted to understand, at the atomic level, how mutations in one of these disease-related proteins, hnRNPA2, would lead to its self-assembly and aggregation.
hRNPA2 plays roles in the processing of RNA — the messenger molecule coding for the production of our proteins — and belongs to a family of proteins also found to be mutated in ALS: hnRNPA1 and hnRNP A2/B1.
Several proteins linked with generative diseases bear a so-called “low complexity” domain. These parts of the protein do not have a static structure, like for rest of the protein, but a rather disordered and flexible shape.
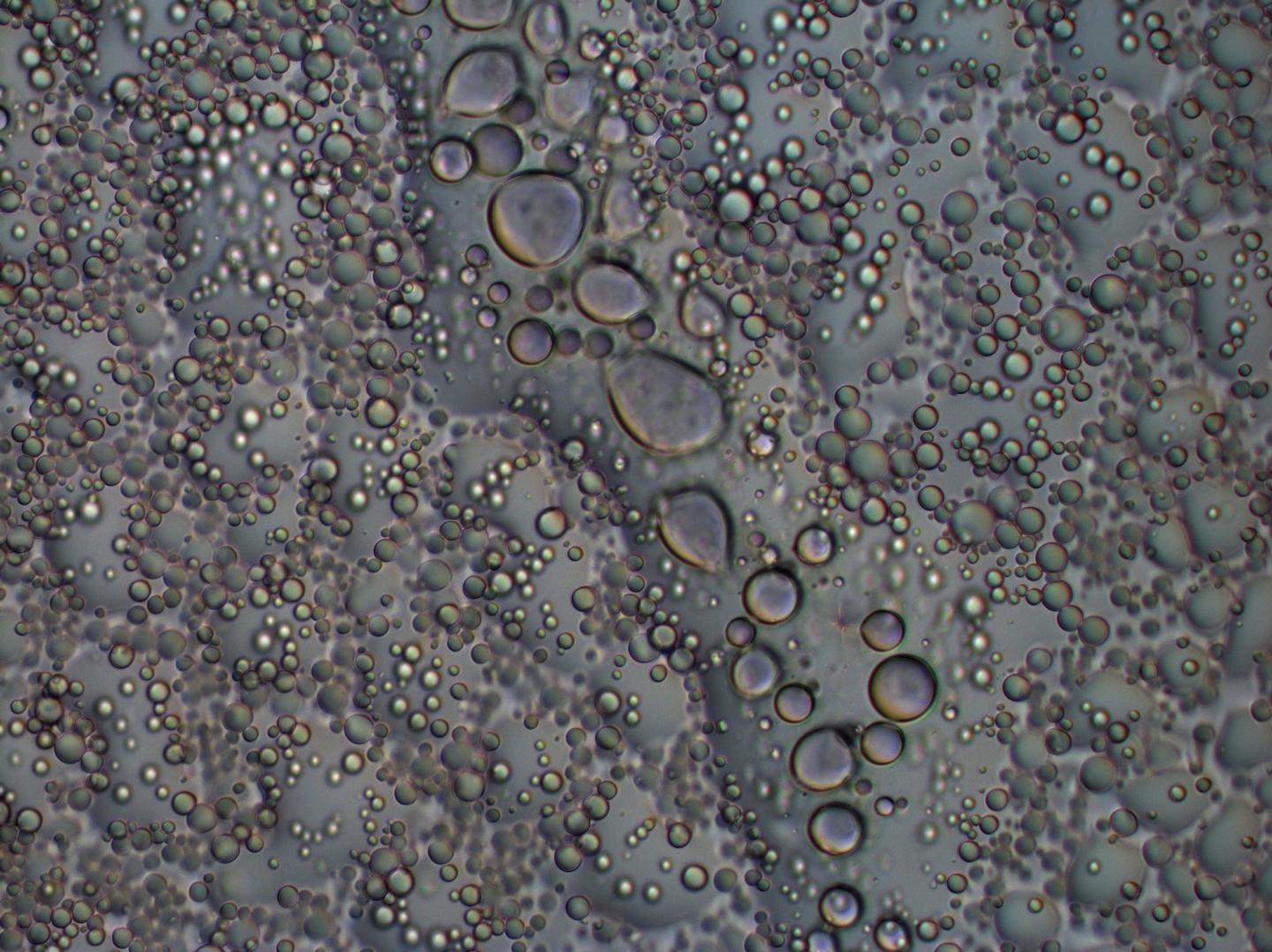
In healthy cells, these protein parts perform important functions such as assembling particular domains called liquid-liquid droplets, where important cellular activities occur.
However, when mutated in the case of ALS or other degenerative conditions, these low-complexity regions start to aggregate and form in-cell inclusions, sometimes even dragging with them other proteins that then begin to function incorrectly.
“We’re trying to understand why they change behavior and aggregate, and how we can disrupt those processes,” Nicolas Fawzi, PhD, the study’s senior author, said in a press release. Fawzi is an assistant professor in the Department of Molecular Pharmacology, Physiology and Biotechnology of Brown University.
Using microscopy, nuclear magnetic resonance (NMR) spectroscopy, and computer simulations, the team compared the physical and chemical interactions in the low complexity domain of healthy and disease-associated hnRNAPA2.
They found that small, atom-level, changes associated with disease can result in bulk changes in the protein organization that result in loss of liquid-liquid separation and aggregation.
“These results highlight the mechanistic role of specific LC [low-complexity] domain interactions and modifications conserved across many hnRNP family members but altered by aggregation-causing pathological mutations,” the researchers wrote.
“We show how small chemical changes — involving only a few atoms — lead to big changes in assembly and disease-associated aggregation,” Fawzi said. “These interactions are more dynamic and less specific than previously thought. A molecule does not take just one shape and bind to one shape but a molecule is flexible and interacts in flexible ways.”
The mechanistic insight brought by the study may help researchers find a way to stop protein aggregation in diseases such as ALS.
“There is currently no therapy or cure for ALS and frontotemporal dementia. We are pursuing new hypotheses and angles to fight these illnesses.” Fawzi said.
“Because these low-complexity domains are too flexible to be directly targeted by standard drugs, finding out how cells use and tame these domains is a potential route to stopping their unwanted assembly in disease,” he concluded.






