Engineered Protein Mutation Prevented Clumping in ALS Motor Neurons
By introducing a mutation in SOD1 — the protein believed to be responsible for a large part of amyotrophic lateral sclerosis (ALS) cases — researchers managed to prevent the protein from clumping in a way that kills neurons.
The study, “A Phosphomimetic Mutation Stabilizes SOD1 and Rescues Cell Viability in 1 the Context of an ALS-associated Mutation,” was published in the journal Cell Structure.
The mutation mirrors a natural tagging of the protein by a chemical phosphate group, providing further support for the notion that both genetic mutations and environmental factors can change the behavior of SOD1 in a way that leads to ALS.
The findings may not only pave the way for the development of drugs that boost SOD1 phosphorylation in patients’ motor neurons as a way to treat ALS, but also allow researchers to look for other ways of stabilizing the protein to prevent it from clumping.
“The identified mutation mimics a natural process called phosphorylation, thus suggesting that there may be a natural, or endogenous, mechanism to stabilize SOD1 in cells and prevent the protein from forming toxic oligomers in people without disease,” Nikolay Dokholyan, PhD, the Michael Hooker Distinguished Professor of Biochemistry and Biophysics at the University of North Carolina, and senior author of the study, said in a news release.
In healthy people, the SOD1 protein form pairs inside cells. Researchers have long known that clumps of the protein are present in motor neurons of patients with ALS, but in a recent study, the research team at Dokholyan’s lab discovered that it was the formation of so-called trimers — gatherings of three SOD1 protein molecules — that produced the toxic effects in nerve cells, ultimately killing them.
Numerous studies have shown that gene mutations, but also changes in how the protein itself is processed, makes it prone to aggregate.
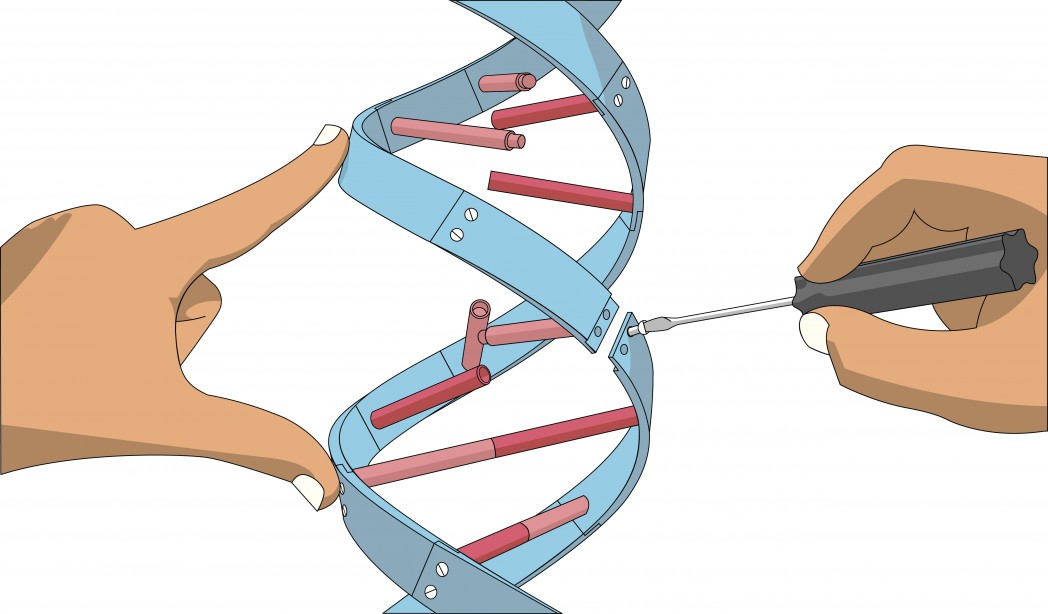
To understand what kind of changes to the protein could help make it more stable, researchers performed computational modeling, which identified a particular protein modification — the placement of a phosphor-tag on a specific site on the protein.
Phosphorylation is a system extensively used throughout the body to alter the behavior of proteins, but for SOD1, it has been difficult to study the effects of such phosphor-tags in the lab.
The research team came up with an alternative solution. They engineered a SOD1 protein with a mutation that mimicked the placement of the phosphor tag. Analyses showed that the mutant looked and behaved just as the naturally occurring protein.
To test if the modification did prevent protein aggregation, the team introduced the mutation in a cell type that already harbored a mutation that caused SOD1 to clump.
“When we transfected this new mutation into cells in concert with the disease mutation, it actually rescued toxicity; it made the cells not die,” said Jimmy Fay, a graduate student in the lab and former lab technician who worked on the research.
“We can now see a way forward,” Fay said. “We know that this mutation stabilizes SOD1, and the hope is that we can find a drug that makes the protein act in this way. By slowly piecing together the larger story of how SOD1 acts, hopefully that can be useful in drug studies to try to get a handle on how to affect the behavior of this protein in a planned way.”