Fat Bubbles May Carry Treatments to Areas of Brain Where They’re Needed
Written by |
Researchers at Columbia University in New York have developed a way to carry treatments for neurological conditions such as amyotrophic lateral sclerosis (ALS) to areas of the brain they would otherwise be unable to reach.
Their targeted approach to overcoming what is known as the blood-brain barrier also reduces the potential for side effects from the therapies affecting other parts of the body, which can happen as treatments travel through the circulatory system.
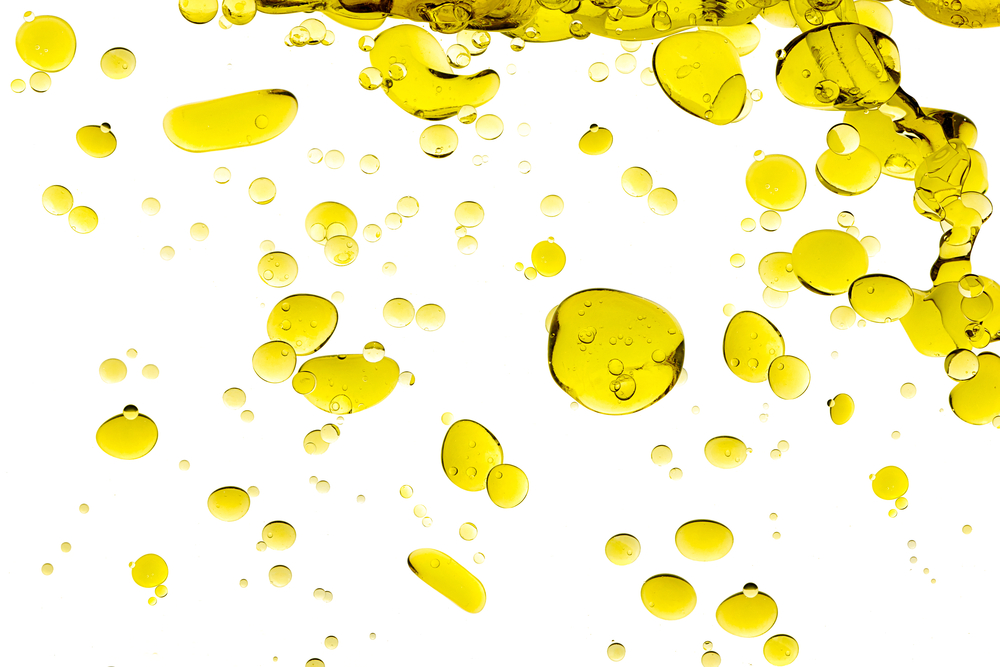
The team, led by Dr. Elisa E Konofagou, embedded the treatments in small fat bubbles, then used ultrasound to oscillate the bubbles, making them bigger.
When the bubbles reached the critical size of eight microns, they were able to open the blood-brain barrier and cross it, allowing the therapies to reach the brain areas where they were needed.
“We’ve made a step forward by incorporating the substance we’re interested in into the lipid (fatty acid) coating of the microbubbles,” Dr. Carlos Sierra, the first author of the study, said in a press release. “This makes the substance stay adhered to the microbubbles and prevents it circulating freely through the body.”
The study, “Lipid microbubbles as a vehicle for targeted drug delivery using focused ultrasound-induced blood-brain barrier opening,” was published in the Journal of Cerebral Blood Flow and Metabolism.
Researchers used a fluorescent molecule, which shows up easily under a microscope, to see if the technique would work in mice. The microbubbles reached the brain without affecting other parts of the animals’ body.
They also identified the level of ultrasound frequency needed for the molecule to reach its target.
The team believes the technique — if successful in tests the researchers are planning to do in monkeys — could be used not only to treat ALS but also other neurological conditions, such as Parkinson’s, Alzheimer’s and Huntington’s disease. It might also treat brain tumors, strokes, and multiple sclerosis.
If it can be adopted to use in patients, the researches believe the technique will lead to better treatments and fewer side effects.
The blood-brain barrier is a defense mechanism that prevents bacteria, viruses, and fungi from reaching the brain. But it blocks neurological therapies as well.
Scientists have had little success with other approaches to the problem, including injecting a treatment directly into the skull, gene therapy, and chemically modifying treatments.