FGF4 shows benefits in ALS but fails to protect motor neurons
Growth factor did reduce activity of star-shaped cells called astrocytes
Written by |
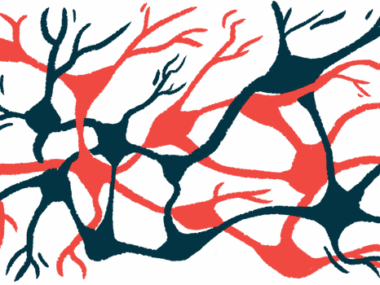
A growth factor called FGF4 can reduce the activity of astrocytes — star-shaped cells in the brain and spinal cord that become overly reactive in amyotrophic lateral sclerosis (ALS) — but it doesn’t stop motor neurons from dying, a study in cells and mice found.
The researchers also observed that the benefits of FGF4 are cut off in the presence of TNF-alpha, a protein that boosts the body’s inflammatory response. This finding suggests that a combination of treatments may be needed to stop or slow disease progression.
According to the team, this study sheds new light on the “complex neuroinflammatory mechanisms at play, involving intricate crosstalk between astrocytes and other cell types,” in ALS. Further research is needed to aid in the development of new therapies for the neurodegenerative disease, per the researchers.
The study, “TNF[alpha] prevents FGF4-mediated rescue of astrocyte dysfunction and reactivity in human ALS models,” was published in the journal Neurobiology of Disease.
Investigating ways to stop motor neurons from dying in ALS
ALS occurs due to the death of motor neurons, the nerve cells that control voluntary movements in the body, which leads to muscle weakness and a range of other symptoms. The exact causes of ALS are unclear, but the transition of astrocytes from supporting to highly reactive is believed to contribute to disease development and progression.
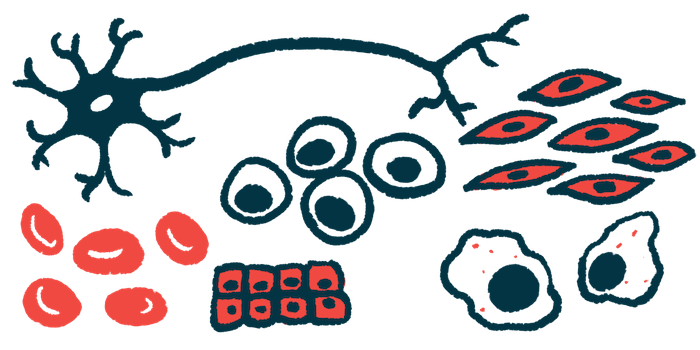
Research shows that astrocytes from people with ALS differ from healthy astrocytes in how they behave and respond to inflammation. Now, an international team of scientists developed astrocytes from human induced pluripotent stem cells (iPSCs) carrying a mutation in the SOD1 gene that’s linked to ALS.
iPSCs are stem-like cells that are derived from mature cells, such as skin or blood cells, and reverse-engineered to take on a stem cell behavior. With the right molecular cues, iPSCs can be matured into any kind of cell in the body, which allows researchers to study diseased cells in the lab without collecting them directly from the affected tissue, such as those in the brain or spinal cord. The resulting cells also carry the exact same genetic alterations as the affected brain cells, which creates a highly accurate model for studying a disease at the cell level.
To reduce the reactivity of ALS-derived astrocytes, the researchers tested various fibroblast growth factors, or FGFs. Among them, FGF4 was found to be the most effective in reversing changes linked to ALS. This suggested that FGF4 could help restore some of the normal astrocyte functions that are lost in ALS.
When FGF4 was injected into the spinal canal of mice with ALS carrying a SOD1 mutation, it also reduced the reactivity of astrocytes. However, treatment with FGF4 did not reduce motor neuron death, suggesting it cannot fully prevent the damage caused by the disease.
Future studies should focus on elucidating these complex interactions and exploring combination therapies to reduce neuroinflammation and enhance neuronal survival, potentially leading to more effective treatments for ALS.
Further research showed that TNF-alpha stopped the benefits of FGF4 on astrocytes. This finding reveals that various inflammatory signals in the ALS environment can make it more difficult for treatments to work effectively.
“Future studies should focus on elucidating these complex interactions and exploring combination therapies to reduce neuroinflammation and enhance neuronal survival, potentially leading to more effective treatments for ALS,” the researchers wrote.
While more work is needed, “this study highlighted the potential of patient-derived iPSC models to capture the cell-autonomous contribution of astrocytes in ALS pathogenesis [disease-causing mechanisms] and to test new therapeutic approaches aimed at modulating astrocyte responsiveness in ALS,” the team concluded.