Gut Microbiome Changes Evident Before ALS Onset, Study Finds
Written by |
A mouse model of amyotrophic lateral sclerosis (ALS) carrying a mutation in the SOD1 gene showed alterations in the gut microbiome, followed by motor impairments and defects in enteric nervous system — the gut’s own autonomous nervous system — compared with healthy mice, a study found.
These microbiome changes occurred early in the disease’s course but eased when the mice were given butyrate, a naturally occurring anti-inflammatory substance produced by certain gut bacteria.
Findings suggest that therapies targeting the gut microbiome could be beneficial to people with SOD1-ALS, its researchers noted.
The study, “Aberrant enteric neuromuscular system and dysbiosis in amyotrophic lateral sclerosis,” was published in the journal Gut Microbes.
Increasing evidence suggests that ALS patients have inflammation in the gut and changes in the composition of gut microbes (the gut microbiome), with lower levels of beneficial bacteria.
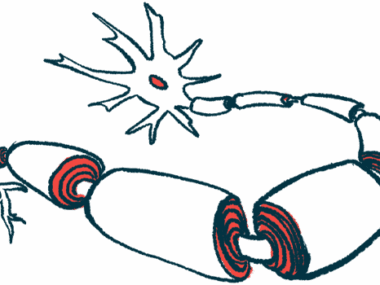
The gastrointestinal tract has its own and independent nervous system, known as the enteric nervous system (ENS). How the ENS and microbiome are affected in ALS, and how they influence disease progression, is unclear.
Researchers at the University of Illinois in Chicago assessed changes in the ENS and microbiome in a mouse model of ALS carrying a mutation in the SOD1 gene. These mice develop symptoms similar to those of ALS patients at about 3 months old. Age-matched normal mice (wild-type) were used as controls.
Changes in intestinal mobility when the mice were at 1, 2 and 3 months of age, were initially assessed. Starting at 2 months old and “before ALS onset,” SOD1-ALS mice had a significantly longer gut transit — the time that ingested food travels through the intestines and is expelled as stool — suggesting a slower intestinal mobility. These 2-month-old mice also had poorer muscle and grip strength.
At the cellular level, ALS mice starting at age 2 months showed changes in protein markers in the intestine. Specifically, a reduction in the smooth muscle myosin heavy chain (SMMHC), a muscle protein, and an increase in glial fibrillary acidic protein (GFAP), a marker of ENS damage, were seen.
These alterations correlated with an increase in the levels of the mutated SOD1 protein in the animals’ intestines.
In a previous study, the researchers found that butyrate, a naturally occurring substance produced by beneficial gut bacteria, improved gut health, delayed the onset of movement symptoms, and increased the life span in mouse models of ALS.
Animals given butyrate in filtered water in this study also showed better motor function and intestinal protein markers relative to untreated animals. Butyrate increased SMMHC protein levels and lowered those of GFAP, and lessened SOD1 aggregation in the animals’ gut. This decrease in SOD1 aggregation was also evident in the lumbar spine of treated mice in this ALS model.
“Butyrate-producing bacteria are known to play an important role in controlling gut inflammatory processes and the maturation of the immune system, primarily through the production of butyrate,” the researchers noted.
Animals given antibiotics, known to change the composition of the gut microbiome, in their drinking water also had better results on motor function tests and healthier levels of muscle and ENS markers than untreated mice.
These findings suggest that “altered intestinal microbiome and function correlate with the skeletal muscle activity and motor neuron function in ALS,” the researchers wrote.
To assess their relevance for patients, the researchers then used human organoids of the colon — stem-cell derived “mini” colons that mimic human tissue in vitro or in lab experiments. The organoids had been manipulated to carry the same SOD1 mutation.
Results showed that feces from the ALS mice promoted SOD1 aggregation in these organoids, while feces from healthy control animals did not.
These findings indicate differences in the microbiome of ALS and control mice, with changes such as a significant enrichment for bacteria with a role in inflammation (Enterohabdus Muris), as well as in bacteria linked with autoimmunity (Clostridium sp. ASF502) evident in between these two animal groups, the study reported.
“The dramatic changes of bacteria in the [SOD1] mice may explain the ability of the feces to enhance SOD1 aggregation in the colonoids,” the researchers wrote.
Changes in the microbiome of ALS mice were rescued with butyrate, suggesting that the benefits of butyrate seen in delaying ALS progression in this mouse model could be mediated by how it affects the microbiome.
“Our study provides insights into the fundamentals of intestinal neuromuscular structure/function and the microbiome in ALS, suggesting the potential to use microbial biomarkers for the diagnosis and to manipulate the intestinal microbiome for the treatment,” the researchers concluded.