Helping Motor Neurons in Spinal Cord Break Down Toxic Proteins as Well as Other Cells Do May Treat ALS, Study Finds
Written by |
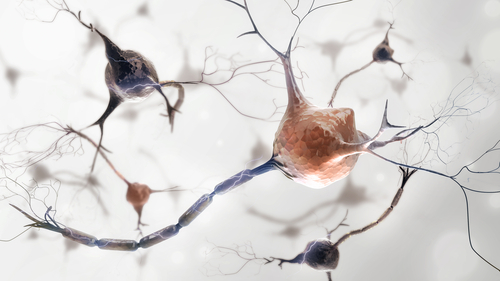
Differences in how efficiently nerve cells degrade and discard proteins may explain why some motor neurons better resist a buildup of toxic proteins than do others in people with amyotrophic lateral sclerosis (ALS), according to a study in mice.
The study, “Stem cell-derived cranial and spinal motor neurons reveal proteostatic differences between ALS resistant and sensitive motor neurons,” appeared in the journal eLife.
Unlike motor nerve cells in the spinal cord, which progressively degenerate throughout ALS, a subset of cranial motor neurons — those that control eye movement — remain functional over much of the disease’s course so as to enable communication via eye-tracking devices. How these cells are able to resist degeneration, however, remains unclear.
One explanation could be the inability of spinal motor neurons to prevent the buildup of toxic protein clumps, possibly due to mutations in components of quality control pathways for proteins in these cells.
Using the human (h)SOD1G93A mouse model of ALS, scientists collected embryonic stem cells (ESCs) to obtain a larger cell population than prior studies addressing this gap. Spinal and cranial motor neurons were obtained by programming the ESCs with specific transcription factors — tiny proteins involved in gene expression — known to drive cell differentiation into these two motor neuron subtypes.
The results showed that resistant cranial motor neurons had fewer misfolded hSOD1 proteins — a typical disease-related alteration in familial ALS — than those in the spinal cord. When the scientists induced an over-production of hSOD1 mutant proteins in vitro (in a lab dish), they found the same differences in misfolding between the two nerve cell types, while also observing that cranial motor neurons were much more efficient in their ubiquitin proteasome system — a sort of cleaning system that degrades and discards misfolded proteins.
These cranial cells also accumulated less p62 (or SQSTM1) protein aggregates over time both in vitro and in vivo (in a living system). Cranial motor neurons were also more resistant to protein damage induced by targeting the endoplasmic reticulum function with stressors called tunicamycin and cyclopiazonic acid. Of note, the endoplasmic reticulum is a key cellular structure in the production, folding, modification, and transport of proteins.
Data further showed that two subsets of ESC-derived cranial motor neurons (oculomotor and trochlear) survived better under stress than spinal cells. Cranial nerve cells also had more proteasome 20S core subunits — known to improve stress resistance — and a higher level of proteasome activity than nerve cells in the spinal cord.
“These unique intrinsic characteristics of [cranial] and [spinal motor neurons] are likely to contribute to their differential vulnerability to ALS neurodegeneration,” the team wrote.
Activating the proteasome by chemical — blocking the p38 MAPK protein — and genetic mechanisms significantly extended the survival of spinal motor neurons experiencing protein stress.
“These findings help elucidate the differences between neuronal types that successfully battle ALS and those that succumb to the disease,” Esteban Mazzoni, the study’s senior author and a professor at New York University’s Department of Biology, said in a press release.
“Having identified a potential mechanism that protects some parts of the body, we are now working on making all neurons ALS resistant,” Mazzoni added. “Specifically, we are striving to identify the different mechanisms that paralyze some parts of the body and leave others fully functional.”