#MDA2022 – NurOwn May Benefit Patients With Specific Gene Variant
Written by |
Treatment with the cell therapy NurOwn may slow the progression of amyotrophic lateral sclerosis (ALS) for those with a specific variation in the UNC13A gene that is linked with a high risk of the disease.
Merit Cudkowicz, MD, chief of neurology at the Massachusetts General Hospital, shared the findings at the Muscular Dystrophy Association (MDA) Clinical and Scientific Conference 2022, in a presentation titled, “Relationship of ALS Genes and Single-nucleotide Polymophisms with Clinical Outcomes in NurOwn Phase 3 ALS Clinical Trial.”
The research was led by BrainStorm Cell Therapeutics, the company developing NurOwn.
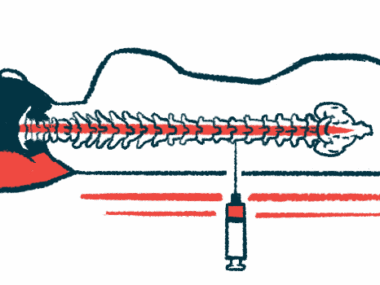
NurOwn is made of mesenchymal stem cells (MSCs) collected from a patient’s bone marrow, which are grown in the lab and matured into cells that produce large amounts of neurotrophic factors – signaling molecules that promote nerve cell growth and survival. These cells are then returned to the patient via a spinal canal injection.
NurOwn’s safety and effectiveness were evaluated in the BTC-002 Phase 3 clinical trial (NCT03280056), which involved 189 people with rapidly progressing ALS. Participants were randomly assigned to NurOwn or a placebo, given directly into the spinal canal every other month for a total of three injections. They were then followed for 28 weeks, about seven months.
The study’s main goal was to assess the number of “responders” to the treatment, defined based on the changes in ALS Functional Rating Scale Revised (ALSFRS-R), a measure of disease severity. Responders were those who showed at least a 1.25-point slower rate of decline in their ALSFRS-R scores than in the 12 weeks leading up to the trial.
Top-line data from the trial showed that the proportion of responders was not significantly different among patients given NurOwn compared with those on a placebo, though some promising trends were seen among patients with early disease.
While ALS is not itself a genetic disease, a number of genetic variations are known to increase the risk of developing it or impact the rate that it progresses. In the Phase 3 trial, 124 participants – 63 on NurOwn and 61 on placebo – underwent genetic analyses.
“This is one of the first studies to prospectively, in ALS, collect DNA and have pre-specified gene mutations” to analyze, Cudkowicz said.
About two-thirds (62%) of the analysis participants were found to harbor an ALS-associated variant in the UNC13A gene, called rs12608932. A pair of recent studies showed that this variation makes the UNC13A gene more susceptible to dysregulation by the abnormal activity of TDP-43.
In ALS, the TDP-43 protein, normally found in the nucleus, forms abnormal clumps in the cytoplasm. The resulting lack of TDP-43 in the nucleus can lead to problems when the UNC13A gene is “read,” particularly in people who carry the rs12608932 variant. As a result, nerve cells make less UNC13A protein, which is important for supporting the health of synapses (connections between nerves).
Since everyone has two copies of the UNC13A gene, one from each parent, each person can have zero, one, or two copies of the rs12608932 variant. Prior research has shown that ALS patients who carry at least one copy of this variant tend to have a shorter survival time, with the worst outcomes being observed in people with two copies.
The researchers examined the rate of responders based on the presence of the rs12608932 variant.
Results showed that there were no differences in responder rates in the overall population in the genetic study (41% for NurOwn vs. 26% for placebo). Responder rates also were similar among patients without the rs12608932 variant (29% vs. 25%) and in those with two copies of the variant (22% vs. 20%) – though Cudkowicz noted that the analyses were limited by the small number of patients with either genotype.
However, in the group carrying one copy of the rs12608932 variant, the responder rate was significantly higher among patients given NurOwn compared with those on a placebo (65% vs. 29%).
Many study participants had low ALSFRS-R scores (i.e., relatively advanced disease) at the study’s start. Among these, Cudkowicz said it’s possible that there was a “floor effect” — essentially, if symptoms are already advanced, it may be hard to detect any improvement from treatment.
When patients with a score of 25 or below at the start of the study were taken out of the analysis, results showed that the response rate for all genotypes (carriers or non-carriers) who received NurOwn stayed the same. The placebo groups with zero or two copies, however, had lower responses than when the overall population was included.”
“Our results suggest that NurOwn treatment may influence disease progression in ALS patients who possess this risk allele and provides a basis for further genetic characterization in clinical trials,” the researchers concluded.
Cudkowicz noted that further research is needed to understand the mechanistic connection between UNC13A variants and the response to NurOwn treatment. Such studies “are just getting started,” she said.
Cudkowicz said the results highlight the importance of collecting genetic data in ALS clinical trials. The researchers’ analyses did not identify differences in treatment response based on ALS-linked variants in other genes, including CAMTA1, MOBP, and ZNF512B, though Cudkowicz stressed that, in many analyses, the number of patients included was small.