Mechanism Underlying Critical Neuron Degeneration in ALS is Revealed
Written by |

In a new study, researchers found the mechanism behind the degeneration of upper motor neurons in the brain, which current evidence has strongly linked to disease progression in patients suffering from amyotrophic lateral sclerosis (ALS). The findings were published in the journal Cerebral Cortex and the study entitled “Corticospinal Motor Neurons Are Susceptible to Increased ER Stress and Display Profound Degeneration in the Absence of UCHL1 Function”.
ALS is a progressive neurodegenerative disease that affects nerve cells (neurons) in the brain and spinal cord. It is characterized by the gradual degeneration of motor neurons that are responsible for controlling voluntary muscles, such as as the ones involved in movement, speaking, eating, and even breathing. It is a fatal disorder for which there is no cure.
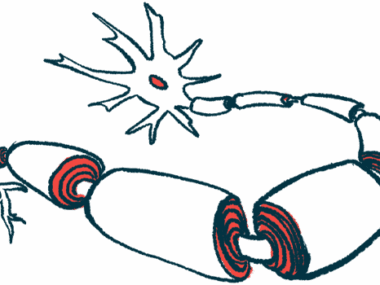
The motor neurons in the brain (called upper motor neurons) transmit messages to the motor neurons in the spinal cord (called lower motor neurons) and subsequently to particular muscles to activate voluntary movement. In ALS, both of these neurons degenerate and die, causing messages to no longer be sent to the muscles. Patients may become totally paralyzed, and a majority of them die from respiratory failure.
“Now that we appreciate the importance of upper motor neurons, we need to develop therapies that improve their survival,” said Dr. Ozdinler, the lead author of the study. “This study gives us a target to go after, bringing us one step closer to building effective treatment strategies.”
The team developed a mouse model to study motor neurons, and discovered that an increase in endoplasmic reticulum (ER – a cellular organelle) stress is responsible for the death of upper motor neurons. In this new mouse model, the animals lacked the UCHL-1 protein, which has been linked to motor defects in humans. The researchers found that the absence of functional UCHL1 protein disturbed ER stress, protein regulation pathways, and the survival rate of upper motor neurons.
“In this model, the timing and extent of upper motor neuron degeneration is unprecedented,” said Dr. Ozdinler. “All the other neurons in the brain remain healthy, which means that this model will be very useful for studying the health of the upper motor neurons.” In addition to the mouse model, the team also developed the first reporter cell line for these neurons that allowed them to visually detect upper motor neurons with the help of a green fluorescent protein.
There are around 2 billion cells in the brain, and of these, only 150,000 correspond to upper motor neurons. “In mathematical terms, they’re insignificant, but their function is so important. They act as the spokesperson of the brain by collecting, integrating, translating and transmitting brain’s message to the spinal cord targets, and by doing so they initiate and modulate voluntary movement,” explained Dr. Ozdinler.
“Now that we have a model and reporter line, we have the tools to develop therapies directed at the upper motor neurons,” said Dr. Ozdinler. “Survival requirements of these neurons cannot be ignored in ALS and in other diseases in which voluntary movement is impaired.”
The team believes their findings could be translated to other neurodegenerative disorders that are ER stress-related. “Parkinson’s, Alzheimer’s and ALS are different branches of the same tree,” added Dr. Ozdinler. “Subpopulations of patients may be developing these diseases due to the same dysfunctional cellular pathways. Finding a therapy for the pathway could help all of these patients.”