Misfolded SOD1 Protein May Have Key Role in Sporadic ALS, Study Suggests
Specific patterns of a misfolded protein — superoxide dismutase 1 (SOD1) — are found in the brain and spinal cord of patients with sporadic amyotrophic lateral sclerosis (ALS), according to a new study, supporting research suggesting that misfolded SOD1 plays a role in this ALS subtype.
The research, “Misfolded SOD1 pathology in sporadic Amyotrophic Lateral Sclerosis,” appeared in the journal Scientific Reports.
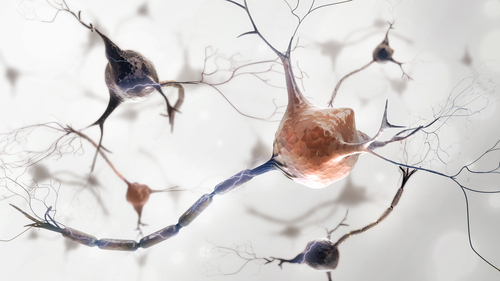
Mutations in approximately 40 genes, including SOD1, have been associated with ALS. Protein misfolding and aggregation in specific regions of the central nervous system characterize neurodegeneration in this disorder.
While its role in ALS is not fully characterized, the SOD1 protein is thought to play an important part in the disease. An over-production of normal SOD1 has been found to cause an ALS-like disease in mice, and SOD1 mutations that produce a similar protein are known to cause ALS.
Researchers have also described the SOD1 protein as able to acquire an abnormal, toxic shape upon oxidative damage, indicating a possible link between sporadic and familial ALS.
But opposing outcomes have been reported in previous research regarding the presence of misfolded SOD1 in patients with sporadic ALS, a point the research team — scientists in Canada and Sweden — attributed to methodological differences. In this study, they used five antibodies that bind to unfolded or misfolded SOD1 to conduct a blinded, standardized analysis in patients with sporadic ALS.
The researchers used postmortem brain and spinal cord tissues from 19 sporadic ALS patients, which were compared to samples from a familial ALS patient with a specific mutation at the SOD1 gene (known as A4V), as well as those from people with Alzheimer’s or without neurological disorders who served as controls.
Using a technique called immunostaining, all five antibodies – which target different parts of misfolded SOD1 – showed clumps of misfolded protein in tissues from the familial ALS patient. This pattern was not seen in the controls with Alzheimer’s or those without neurological disorders, confirming the antibodies’ specificity.
Interestingly, studying tissues from 13 of the sporadic ALS patients, the researchers found that misfolded SOD1 had five specific patterns, including ring-like structures, and deposits of misfolded SOD1 in the cytoplasm, nerve fiber or axonal extensions, and nuclei of motor neurons.
These findings were later confirmed using a different procedure, called immunocapture, in spinal cord samples from the six remaining sporadic ALS patients and the familial ALS case.
The small ring-like structures of misfolded SOD1 found in ALS patients could be corpora amylacea, which are small masses of unknown origin also found in normal aging, as well as in Alzheimer’s and multiple sclerosis, the investigators said.
“Our data are in favour of their specific character in SALS [sporadic ALS] and encourages to consider them as positive marker of the disease even if further studies are necessary in order to clearly delineate their role and their specificity in ALS,” they wrote.
“This blinded, standardized and unbiased approach provides further support for a possible pathological role of misSOD1 [misfolded SOD1] in SALS,” the researchers concluded.






