MSC transplants found to extend survival by 4 years in ALS: Analysis
Trial data show 4 patients alive, with one at more than 20 years survival
Written by |
Transplants using mesenchymal stromal cells or MSCs — a type of stem cell found in bone marrow — delivered into the spinal canal can significantly extend survival in people with amyotrophic lateral sclerosis (ALS) compared with what would be expected based on their clinical characteristics, a new analysis of trials from the early 2000s found.
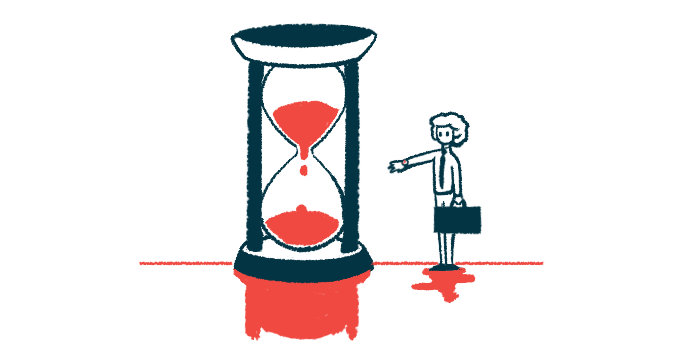
In two Phase 1 clinical trials that tested such stem cell transplants, the median time patients lived without requiring permanent ventilatory support was about 118 months, or nearly 10 years — about four years longer than the roughly 70 months of predicted survival time — pooled study data show.
At the time of the analysis, four patients (about 20% of participants) were alive, including one with a predicted survival of 91 months (about 7.5 years) who was alive at 303 months without needing a breathing or feeding tube. In other words, the patient was alive more than 20 years later.
“The current study represents the first very long-term analysis of survival as an effect of MSC focal transplantation in the central nervous system [brain and spinal cord] of ALS patients, demonstrating that MSC transplantation could potentially slow down ALS progression and improve survival,” the researchers wrote.
The study, “Effect of mesenchymal stromal cell transplantation on long-term survival in amyotrophic lateral sclerosis,” was published in Cytotherapy.
Original trials involving these stem cell transplants conducted in 2002 and 2006
ALS is a rare neurodegenerative disease marked by the progressive loss of motor neurons, the nerve cells that control voluntary movements. There is no cure to date, and few effective treatments are available to slow disease progression.
MSCs, also called mesenchymal stem cells, are a form of stem cells that can give rise to several connective tissue cells, such as fat cells and blood vessel cells.
These cells also can produce a range of signaling molecules that modulate immune responses and have tissue-protective and regenerative properties. As such, their use is considered a potentially promising approach for treating ALS.
The safety and feasibility of transplanting MSCs into the spinal canal has been established in ALS clinical trials. But few studies have reported the long-term effects of these cells in patients.
To address that, and eventually support a Phase 2/3 trial, researchers in Italy examined the long-term outcomes of ALS patients treated with MSCs in clinical trials conducted in the early 2000s. Specifically, the two Phase 1 clinical trials reviewed here were conducted by the team in 2002 and 2006.
Nineteen patients were treated in these studies, with nine involved in the first trial and 10 in the second.
For each patient, the team calculated survival — defined as time to permanent non-invasive ventilation, breathing tube, or death — using the European Network to Cure ALS (ENCALS) model. This tool predicts survival based on certain clinical characteristics, including age at disease onset, lung function, any delay in diagnosis, the rate of disease progression, and the presence of certain ALS-related mutations.
The expected survival for each patient based on this model was then compared with the individual’s actual survival time.
The results showed MSC treatment significantly extended the patients’ lives compared with what would be expected based on their clinical characteristics. While the ENCALS model estimated a median survival of 70.8 months, patients actually lived for 118.8 months on average — four more years than estimated.
The current study represents the first very long-term analysis of survival as an effect of MSC focal transplantation in the central nervous system [brain and spinal cord] of ALS patients, demonstrating that MSC transplantation could potentially slow down ALS progression and improve survival.
Of the total 19 patients, 13 (68%) had a longer survival time than expected. One patient had been classified as having a short survival and transitioned to intermediate, and three were intermediate and ended up having a long-to-very-long survival. The other nine were classified as very long survival, but still ended up living for more months than expected.
The survival extension was particularly evident in a group of patients with slow disease progression, 80% of whom lived longer than expected. Among those with fast progression, only 55% had longer survival than estimated; the other 45% lived less time than expected.
At the time of the analysis, four patients were still alive, including one who started noninvasive ventilation 35 months (nearly three years) after treatment and one who is still living without the need for ventilatory support. The other two patients have required a tracheostomy — a procedure in which a tube is fitted through a hole in the neck to help with breathing.
Together, these results show a potential for stem cell transplants with MSCs to slow disease progression and improve survival in ALS patients, providing “new insights for planning the next generation of efficacy MSCs clinical trials in ALS,” the researchers wrote.
The team noted that stem cell transplantation’s role in ALS still needs further understanding. But the researchers hypothesized that “the observed clinical effects could be primarily based on modifying the extra-motor neuron environment, such as through the release of trophic factor and the modulation of neuroinflammation.”