Results Published From Phase I Trial on Human Neural Stem Cell Transplantation in Patients With Amyotrophic Lateral Sclerosis
 Results from a recent Phase I clinical trial in patients with Amyotrophic Lateral Sclerosis (ALS) showed a safe cell therapy approach that may allow for the treatment of larger pools of patients for later-phase ALS trials. The study is published in the Journal of Translational Medicine.
Results from a recent Phase I clinical trial in patients with Amyotrophic Lateral Sclerosis (ALS) showed a safe cell therapy approach that may allow for the treatment of larger pools of patients for later-phase ALS trials. The study is published in the Journal of Translational Medicine.
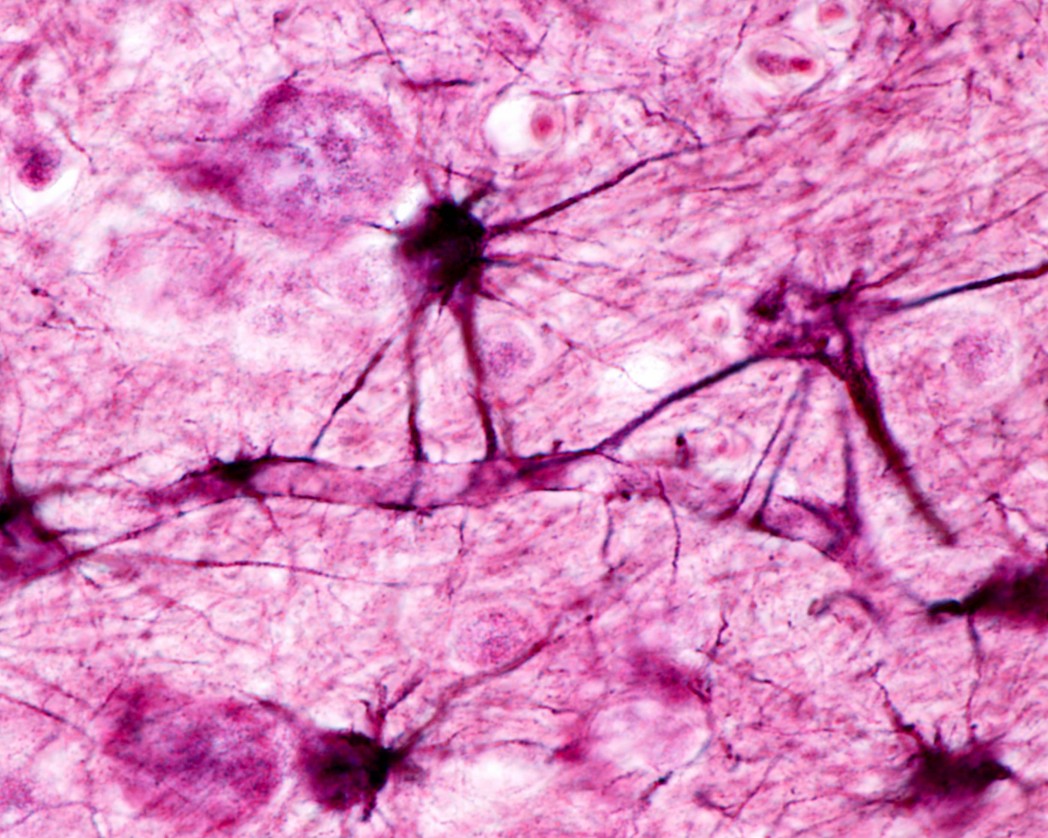
Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disease that targets motor neurons (MNs) in the primary motor cortex, brainstem, and spinal cord. Cell therapy is emerging as a potential therapeutic option in ALS, although there are concerns related to the type of stem cells to be used in cell therapy for ALS. Studies using both hematopoietic and mesenchymal stem cells (MSCs) have now been transplanted into the spinal cord of ALS patients, in the absence of long-term negative effects.
Other studies have shown the integration capacity and efficacy of human neural stem cells (hNSC) in preclinical rodent models of neurological diseases.
In the article entitled “Human neural stem cell transplantation in ALS: initial results from a phase I trial,“ Letizia Mazzini from the Department of Neurology, Eastern Piedmont University, Maggiore della Carità Hospital in Italy and colleagues report the preliminary results from a first group of six ALS patients in an ongoing Phase I trial, in which bona fide, multipotent hNSCs were isolated and reproducibly expanded from human fetal tissue.
In the study, patients were treated either with 3 unilateral hNSCs microinjections into the lumbar cord tract (N=3) or bilateral (n = 3 + 3) microinjections (N=3). There were no major severe side effect observed associated to the treatment.
The results showed that after 18 months of follow-up after surgery, there was no increase in the progression of the disease because of the therapy. In two patients there was an improvement of the subscore ambulation on the ALS-FRS-R scale (from 1 to 2). In a third patient the results revealed an increase of the MRC score for tibialis anterior, persistent for 7 months.
The latter patients in the study rejected PEG and invasive ventilation and died 8 months following surgery due to respiratory failure. Results from the autopsies established that the deaths were related with the disease’s progression.
Based on the results, the researchers indicate that this cell therapy approach may allow for the treatment of larger pools of patients for later-phase ALS clinical trials. Importantly, the researchers point out that a trial can now be carried out under standardized conditions, based on a consistent selection of hNSCs. They also state the fact that using brain tissue from natural miscarriages disregards the ethical issues related to the use of fetal material.