Scientists find promising 3 drug combo for sporadic ALS using new models
Successful screening 'a major milestone for drug discovery,' researchers say
Written by |
- Newly developed cell models of sporadic ALS, found to accurately reflect disease features, may aid in drug discovery.
- A triple drug combination showed promise in these models for treating ALS in people with no family history.
- A lack of reliable models had slowed the development of new treatments for sporadic ALS.
A triple combination therapy has shown promise for treating sporadic amyotrophic lateral sclerosis (ALS), according to a new study that used cell models of the disease to screen more than 100 therapeutic compounds.
The new cell-based model was created from motor neurons, or nerve cells, derived from people with sporadic ALS. Extensive analyses showed that the model recapitulated the features of motor neuron degeneration seen in people with this disease type — individuals who have no known family history of ALS.
The three drugs have all been previously tested in ALS clinical trials, the researchers noted.
“The successful screening and preclinical testing of drug efficacy across the [sporadic ALS] population represent a major milestone for drug discovery in ALS and removes a major roadblock for therapeutic development,” the team wrote.
The study, “Large-scale drug screening in iPSC-derived motor neurons from sporadic ALS patients identifies a potential combinatorial therapy,” was published in the journal Nature Neuroscience. by scientists in Australia.
A progressive disease, ALS is characterized by the loss of motor neurons, the nerve cells in the brain and spinal cord that control movement. About 10% of patients have familial ALS, in which at least one family member has the condition, while most have sporadic ALS with no family history.
Lack of models has slowed new therapies for sporadic ALS
While familial ALS has been linked to mutations in about 40 genes, the vast majority of sporadic ALS cases have no known cause. Due to a lack of reliable animal or cell-based models that accurately represent sporadic ALS, it has been difficult for scientists to identify the core mechanisms driving this form of the disease.
That has limited the development of targeted therapies, according to the researchers.
“Developing pathophysiologically relevant models of [sporadic ALS] for drug development and preclinical testing remains a core challenge in ALS research,” the scientists wrote. Pathophysiology refers to the functional, biochemical, and structural changes that occur in the body as a result of disease.
Now, a group of Australian researchers, led by scientists at The University of Melbourne, created cell-based models of this common ALS type.
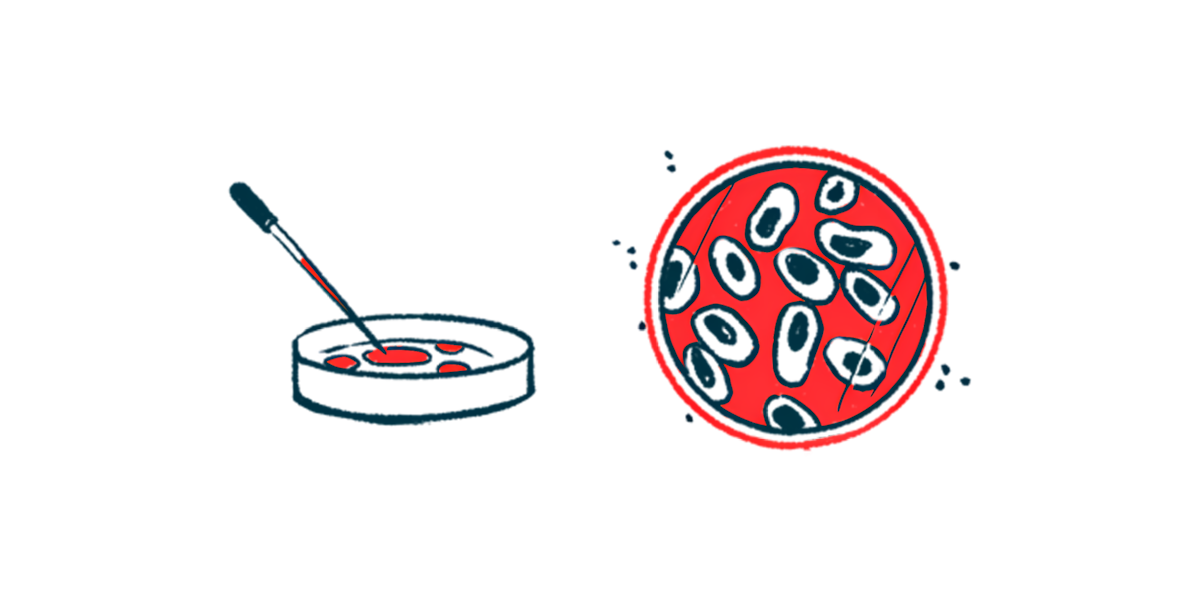
To create the models, the team first collected skin cells from 100 sporadic ALS patients, 11 suspected familial ALS patients, and 25 controls without neurodegenerative diseases. Cells were reprogrammed into a stem cell-like state, called induced pluripotent stem cells (iPSCs), and subsequently differentiated into mature motor neurons.
To validate the models, the team assessed the survival of patient-derived motor neurons by measuring the time it took for neurites — the hair-like projections that extend from the nerve cell body — to shrink by 50% (LD50). Neurite shortening is a sign of neurodegeneration.
The LD50 survival time for motor neurons derived from both familial and sporadic type patients was significantly shorter than that of controls, indicating reduced survival.
Further, a reduced LD50 of these motor neurons matched a shorter survival time of ALS patients as well as a faster disease progression, “supporting a link between patient-derived motor neurons and clinical prognosis,” the team wrote.
Additional experiments revealed that gene activity patterns in patient-derived motor neurons closely matched those in postmortem spinal cord samples from people who had sporadic ALS.
“These results support the idea that motor neurons derived from patients with [sporadic ALS] can recapitulate the [disease-related] processes occurring in the motor neurons of patients,” the team wrote.
Researchers use models to test over 100 drugs
Finally, the team used the cell models to test 107 drugs that had been previously evaluated in clinical trials for ALS. Nearly all of the drugs tested (97%) failed to improve the health of motor neurons derived from 16 sporadic ALS donors.
However, three medications — riluzole (which is already approved for ALS as Tiglutik and generics), baricitinib, and memantine — demonstrated efficacy over time, the data showed.
The successful identification and preclinical validation of three-drug combinations using patient-derived [sporadic ALS] motor neurons demonstrate the power of [the new cell models] to measure drug efficacy across [this] patient population and represent an important milestone in drug development for ALS.
When tested directly for LD50 survival, significant improvements in motor neuron health were observed for riluzole and baricitinib, but not for memantine. Still, combining two or all three medicines significantly increased LD50 survival, with the triple combination showing the greatest benefits, according to the researchers.
“The successful identification and preclinical validation of three-drug combinations using patient-derived [sporadic ALS] motor neurons demonstrate the power of [the new cell models] to measure drug efficacy across [this] patient population and represent an important milestone in drug development for ALS,” the researchers wrote.