Way of Preventing Harmful Protein Clumping Seen in ALS Raised in Early Study
Proteasome, a cellular component, plays a key role in the maintenance of proper levels of proteins inside cells. Two researchers at the Massachusetts General Hospital (MGH) have identified, through studies in a roundworm, key molecules in the pathway through which cells sense and repair proteasome abnormalities. Such findings may lead to new therapies for many diseases, including neurodegenerative diseases such as ALS, that are characterized by aberrant protein aggregation.
The research paper, titled “Proteasome dysfunction triggers activation of SKN-1A/Nrf1 by the aspartic protease DDI-1,” was published in eLife.
The proteasome degrades unnecessary and defective proteins to maintain adequate levels and a balance of proteins within cells. When proteasome stops working as it should, cells respond by increasing the production of its components in an attempt to prevent a harmful accumulation of proteins, which can result in disease.
“Boosting proteasome activity might help treat some neurodegenerative disorders — including Alzheimer’s and Parkinson’s disease, both of which are characterized by abnormal protein deposits in the brain that exceed the ability of the proteasome to respond,” Nicolas Lehrbach, PhD, the study’s lead author, said in a news release.
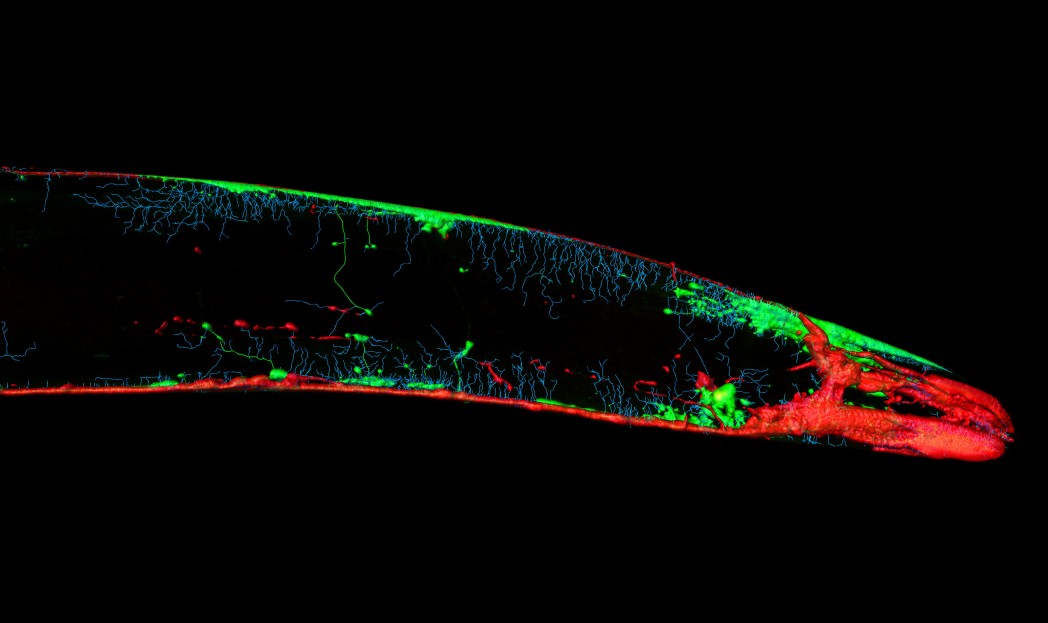
Previous research in the C. elegans roundworm found that the transcription factor SKN-1 is essential for this cellular response to proteasome abnormalities, but the exacts mechanism by which SKN-1 induces expression of proteasome components remained unknown.
Here, the researchers did a genetic screen of C. elegans mutants unable to activate SKN-1 in order to spot the mutated genes. Through this, they identified nearly 100 new mutations that make these animals unable to sense and respond to proteasome dysfunction. Among the mutations was DDI-1, a protease enzyme, and the protein PNG-1.
Researchers found that SKN-1 activation is dependent on cleavage or clipping by PNG-1, and PNG-1 removal of a sugar molecule. Transcription factors Nrf1 and Nrf2 are the mammalian versions of SKN-1, and blocking Nrf1 has been proposed a way of improving protease inhibitor treatment of cancer.
A different study, conducted by researchers at the University of Tokyo, found that DDI-2, the human version of DDI-1, is necessary for the response to proteasome deficiency in human cells. Both studies point to the importance of DDI-1/2 protease for the sensing of proteasome stress in animals, from roundworms to humans, which suggests that the enzyme is an ideal target for drug development.
“We know from the successful development of protease inhibitors to treat HIV and hepatitis C infection that protease enzymes are highly amenable to the development of small-molecule inhibitors,” said Gary Ruvkun, PhD, of the MGH Department of Molecular Biology and corresponding author of the study.
“In addition to potentially being powerful enhancers of the proteasome inhibitors being used to treat multiple myeloma, DDI-1/2 inhibitors may be more generally deployed against conditions in which proteasome deregulation has been implicated — for example, the variety of diseases caused by aberrant protein aggregation, such as Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, amyotrophic lateral sclerosis, and prion diseases,” he added.






