Genetic ALS: Discussing a difficult diagnosis

Perspective from Robert Bucelli, MD, PhD
Dr. Robert Bucelli is a professor and neurologist at Washington University in St. Louis. He consults and cares for many people with ALS at the school’s world-renowned ALS Center. Dr. Bucelli is a paid consultant for Biogen and was compensated for this article.
One of the most challenging parts of my job is having to give someone the diagnosis of ALS.
Providing a diagnosis of ALS is a very personalized experience, and I feel it’s my responsibility to adapt to that. People with ALS have varying perspectives that influence how they approach their illness. It’s up to me and my fellow doctors to remain open to those perspectives.
 Being in my patient’s corner
Being in my patient’s corner
Every doctor is taught how to handle these types of discussions, but what is learned in the classroom is never quite what is experienced in real life. This is an incredibly emotional moment and emotions are very unpredictable.
Receiving a diagnosis of ALS is never easy. I’ve seen people experience everything, from anger to sadness to devastation to denial. Many times, I find that my patients and their caregivers might be unable to process anything being discussed in the moment beyond the diagnosis itself.
On the other hand, some of my patients are immediately engaged and eager to learn everything they can. They may want to talk about possible next steps within minutes of receiving the diagnosis. In these cases, it is important that I match their level of interest and engagement. It is equally important to note that, no matter how many times I do this, it is difficult. But the vast majority of the people I treat benefit from knowing their diagnosis as early as possible.
 Genetic counseling and testing are important1
Genetic counseling and testing are important1
The relationship between genetics and ALS has become an essential part of conversations with my patients.
I typically discuss genetic testing at the first or second visit, and sometimes my patient might be the first one to bring it up. They may have learned that there may be a link between genetics and ALS. I generally quote a statistic that approximately 15% of people with ALS have a disease-causing mutation in an ALS gene, even in the absence of a clear family history of ALS.2,3 I believe that some background on basic genetics as well as the genetics of ALS is helpful, but I also feel that a discussion with a genetic counselor is essential.
Genetic counseling may come into play both before genetic testing is done, in order to know what to expect, and afterwards, in order to help understand and interpret the results.1
 Empowering with knowledge
Empowering with knowledge
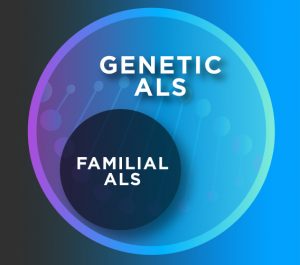
I worry that some people react negatively to terms like “hereditary ALS” or “familial ALS.” I prefer to avoid these phrases altogether. They can make some people fearful or even feel guilty, like they may have done something to hurt a loved one or vice versa.
Emerging knowledge shows that not everyone with genetic ALS, or ALS associated with an identified genetic mutation, has a family history of the disease. Additionally, not everyone with a family history—or even everyone who carries a genetic mutation—will develop ALS.1 I try to reassure patients that there is absolutely nothing they have done wrong. Genetic ALS is associated with their biology. It is not within their control.
My conversations with my patients also include information about what it means if no mutation appears in their results. Some testing panels may not include all known mutations. Also, new discoveries continue to be made—a gene that can cause a person’s ALS may not yet have been identified.4
 Genetic testing has drawbacks and benefits
Genetic testing has drawbacks and benefits
It is important to note that genetic testing can inform multiple aspects of care. For example, a certain genetic outcome may result in eligibility to participate in a clinical trial. But it is important to take family dynamics into account, as some family members may want to know about their genetic risk while others may not. I generally do not suggest that my younger patients, such as those under the age of 18, get a genetic test if they are asymptomatic.
Genetic testing has implications for the broader ALS community as well, and can affect the course of ALS research. Based on my experience, I have found that there are also individuals who undergo genetic testing because they are committed to furthering disease knowledge for the benefit of the overall ALS community.
Learn more about genetic ALS by visiting insideALS.com from Biogen.
©2021 Biogen. All rights reserved. 225 Binney Street, Cambridge, MA 02142 04/21 ALS-US-0042