Researchers Identify Culprit in ALS Nerve Cell Damage, Potentially Leading to New Therapies
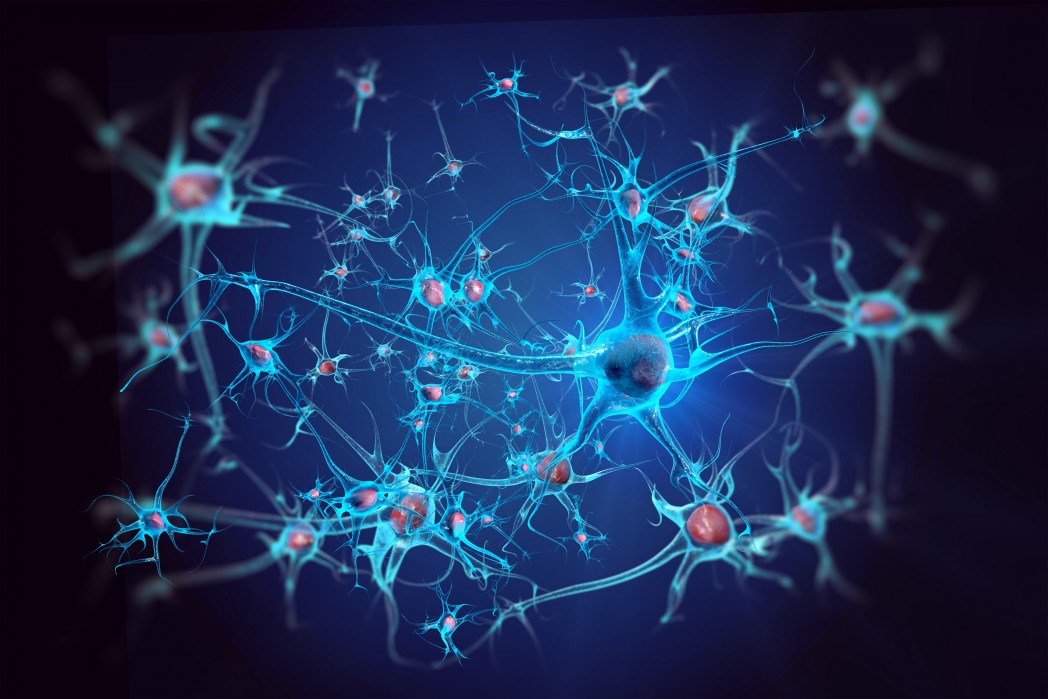
Researchers at Harvard Medical School have made an important breakthrough in amyotrophic lateral sclerosis (ALS) research, identifying an enzyme that plays a key role in the demise of nerve cells in ALS patients and paving the way for research in new therapies.
Their discovery has already set in motion the development of new treatments for humans after researchers were able to stop nerve cell damage in mice.
The research paper, “RIPK1 mediates axonal degeneration by promoting inflammation and necroptosis in ALS,” was published in the journal Science.
The study’s senior investigator, Junying Yuan, the Elizabeth D. Hay Professor of Cell Biology at Harvard Medical School, and his team have investigated the enzyme RIPK1 over the last decade, discovering its key role in inflammation and cell death.
But it wasn’t until recently that researchers connected the enzyme to nerve cell damage and ALS. The study reveals that RIPK1’s abnormal behavior leads to the disruption of the production of myelin, the substance that envelops axons — the neuron’s projections that transmit signals from one cell to another — and protects them against damage.
The researchers conducted experiments in mice and human ALS cells and found that when the enzyme is out of control, it can set off a chemical reaction that eventually leads to the demise of the protective myelin and, consequently, damage to the axons, a hallmark of ALS. The targets of RIPK1 are the cells responsible for the production of myelin, nerve cells called oligodendrocytes.
In previous research, the team showed that the activity of RIPK1 could be blocked by a chemical called necrostatin-1. Building on this knowledge, researchers tested how mice who had been modified to develop ALS would respond to this chemical, and found that it tamed the activity of RIPK1. The researchers also used necrostatin-1 to treat mice with axonal damage and leg weakness, a sign of axonal damage similar to the muscle weakness that is observed in ALS patients. The chemical restored the myelin sheath and stopped axonal damage and also prevented limb weakness in the animals treated with it.
Additional experiments revealed that a lack of the optineurin (OPTN) gene, previously connected to both inherited and sporadic forms of ALS, was directly involved in the nervous system’s inability to produce myelin. In their search for an explanation, the scientists found abnormally high levels of RIPK1, which promotes cell death, in spinal cord cells from mice lacking OPTN. These findings led researchers to conclude that the OPTN gene may regulate the behavior of RIPK1 by ensuring its levels are normal and the enzyme is correctly processed.
To further explore the scope of RIPK1 influence, researchers also examined neurons obtained from mice with the most common inherited form of ALS, the one caused by mutations in the SOD1 gene, and observed that RIPK1 was also elevated in these cells.
In light of this, researchers theorize that OPTN may not be the only gene regulating RIPK1’s behavior and that the enzyme may lead to axonal damage in various forms of inherited and acquired forms of ALS, as well as other neurodegenerative diseases.
“Our study not only elucidates the mechanism of axonal injury and death but also identifies a possible protective strategy to counter it by inhibiting the activity of RIPK1,” Yuan said in a news release.