Spinal Fluid and Blood Proteins May Diagnose and Predict Outcomes in ALS, Study Finds
Specific proteins analyzed in cerebral spinal fluid and blood samples may help to diagnose amyotrophic lateral sclerosis (ALS) and predict patient outcomes, researchers report.
Cerebral spinal fluid (CFS) protein patterns helped to identify 94% of ALS patients in their study, and the levels of three specific proteins were seen to explain 49% of variation in their degrees of physical disability.
The study, “Machine Learning Reveals Protein Signatures in CSF and Plasma Fluids of Clinical Value for ALS,” was published in the journal Scientific Reports.
Because the underlying progressive mechanisms of ALS are not fully clear, expected outcomes for patients often rely on early diagnosis and prompt treatment with approved therapies to slow or prevent disease progression.
But no molecular biomarkers are known to accurately diagnose and predict ALS progression. And a diagnosis may only be reached one to two years after symptom onset, because ALS symptoms mimic other disorders and its characteristic signs, such as upper and lower motor neuron deterioration, are often not evident immediately.
“A lot of time and money gets spent by patients during that time period. And once a patient has a diagnosis, the tools we currently have to monitor disease progression are very subjective,” Michael Bereman, an ALS patient, an assistant professor in biological sciences at North Carolina State University, and the study’s lead author, said in a university news story written by Tracey Peake.
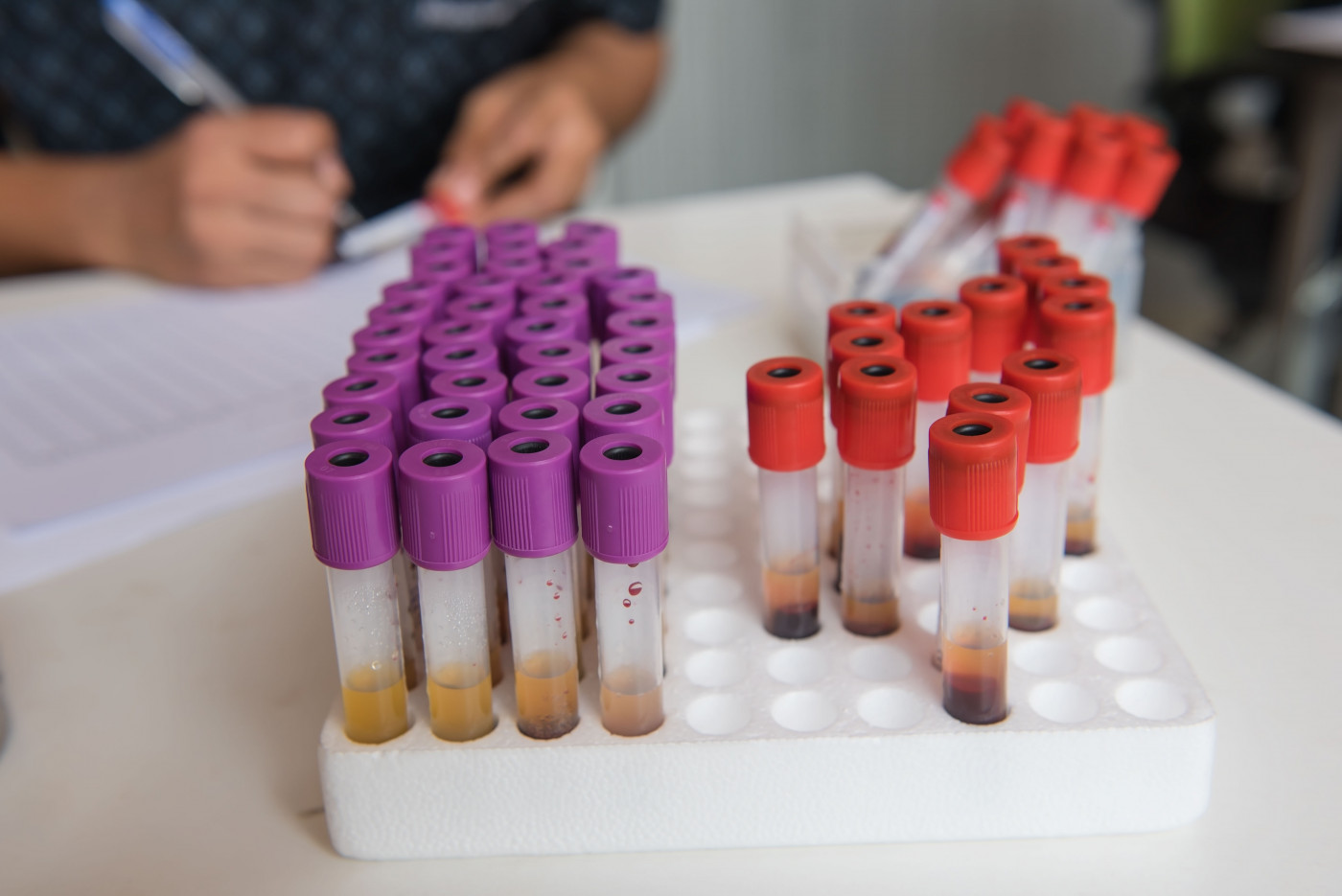
Researchers conducted a broad analysis of protein content in cerebrospinal and plasma fluid samples collected from 33 ALS patients and 30 healthy volunteers, searching for potential biomarkers of ALS.
They found 118 proteins in CSF samples and 20 proteins in blood samples that significantly differed between patients and healthy controls. “The small number of significant proteins found in the plasma samples is most likely due to its distal nature, large dynamic range of plasma proteins, and both intra and inter-individual protein variability,” the researchers wrote, later adding, “CSF proved most fruitful.”
Ten proteins were found to differ the most, and all had been previously linked with one or more neurodegenerative diseases, including ALS. In addition, many of the altered proteins in CSF samples were related to signaling pathways previously shown to be altered in ALS patients, including the activation pathway of the immune complement system and the retinoid signaling pathway.
In particular, researchers found a positive correlation between complement component 7 (C7) and retinol binding protein 4 (RBP4) in both CFS and plasma samples from patients, and “an insignificant negative correlation”in those from controls.
“While the biological significance of this observation is unclear, these results do suggest a systemic [organism-wide] or even coordinated role of C7 and RBP4 within and outside the central nervous system in ALS,” the researchers wrote. “These markers could act as a plasma proxy for [ALS therapeutic] intervention.”
Using the collected protein data, the team developed a method of computer analysis that identified 94% of ALS cases. Among the proteins with greater diagnostic potential were chitinase-3 like 1 and alpha-1-antichymotrypsin.
“Our goal is to create a panel of protein targets that could give doctors a quicker path to diagnosis for ALS patients, as well as an objective way to measure disease progression, or to test the efficacy of new drugs,” said Bereman, who is also leader of the proteomics core at NC State’s Center for Human Health and the Environment. Proteomics is the study of proteins and their function.
Researchers also developed a computer algorithm that could explain 49% of the differences seen among patients’ scores in the ALS Functional Rating Scale, a 12-question survey of daily life activities. Proteins identified as having greater prognostic potential here were chitinase-3 like 1, alpha-1-antichymotrypsin, and complement factor 1.
“Our results confirm a previous study that demonstrated that chitinase-3 like 1 protein levels [also known as YKL-40] were correlated with survival in ALS,” the researchers wrote. “However, results described herein indicate that a multi-protein model will improve upon the prognostic value of chitinase-3 like 1.”
The team is planning to further explore the role of these identified proteins and their signaling pathways over time in fluid samples from ALS patients, Bereman said.
“In addition to diagnostic markers, objective measures of prognostic value in ALS would be transformative,” the study concluded.






