Gut Microbiome May Help Slow ALS Progression, Study Indicates
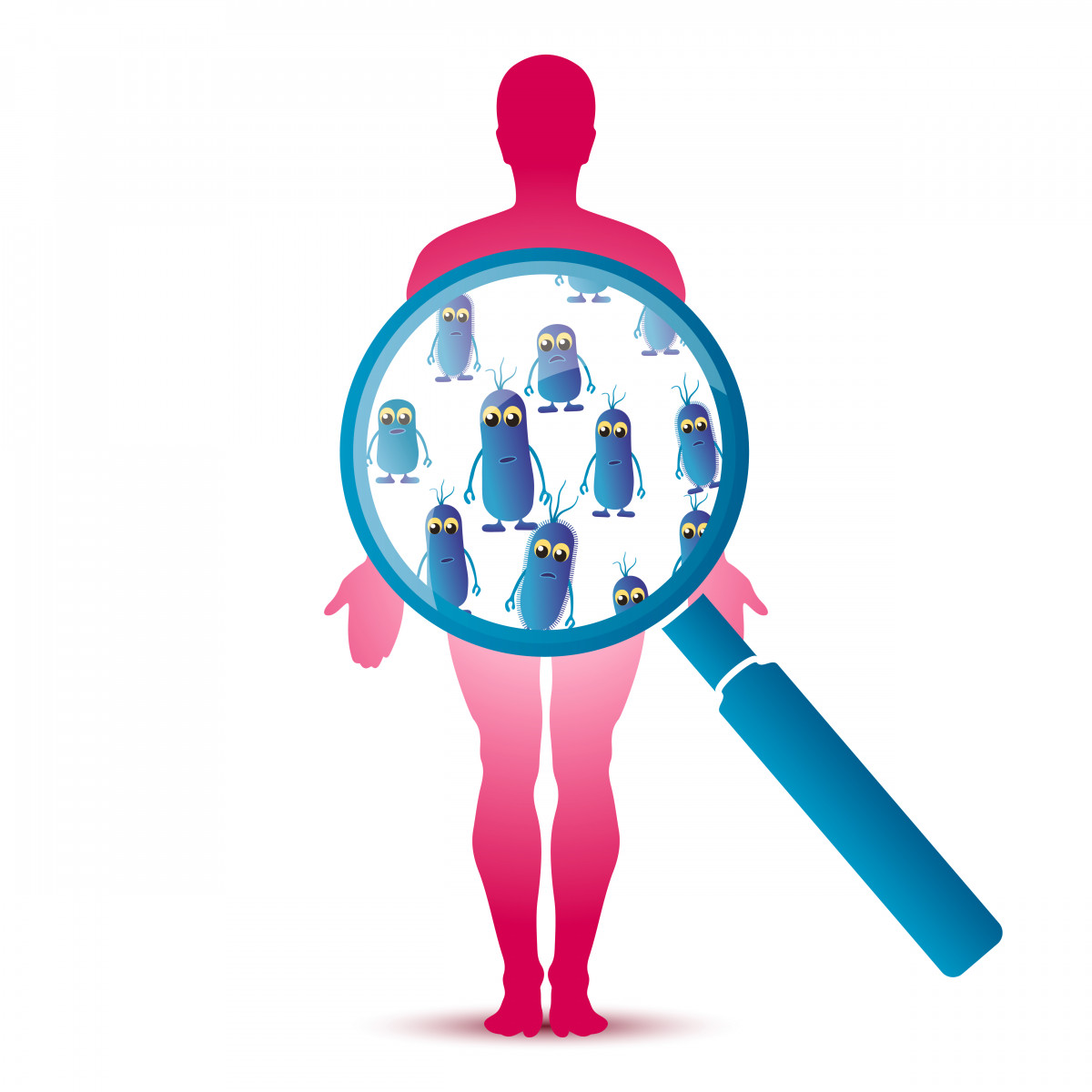
The gut microbiome — the natural collection of microorganisms living in our guts — might influence the progression of amyotrophic lateral sclerosis (ALS), recent research suggests.
Specifically, researchers found that a metabolite produced by the Akkermansia muciniphila bacteria, called nicotinamide, slowed disease progression and prolonged survival in an ALS mouse model. In the future, researchers may harness these metabolites to slow or even halt ALS.
The study, “Potential roles of gut microbiome and metabolites in modulating ALS in mice,” was published in the journal Nature.
ALS is a neurodegenerative disease in which motor neurons die prematurely. The exact cause is still unknown, but researchers believe it is a mix between genetic and environmental factors.
The human gut microbiome is increasingly recognized as a key factor determining the susceptibility to certain diseases, including those of the brain, and responses to therapy.
Researchers at the Weizmann Institute of Science hypothesized that metabolites originating in the gut could travel through the blood into the brain and affect the function of neurons and other brain cells.
“Given increasing evidence that microbiome affects brain function and disease, we wanted to study its potential role in ALS,” professor Eran Segal, PhD, one of the study’s co-lead authors, said in a press release.
They first investigated what would happen if the microbiome was removed from a mouse model called SOD1-Tg, which mimics ALS. This was achieved by treating the animals with large spectrum antibiotics — the treatment wipes out a significant part of the gut microbiome — or by growing the animals in germ-free conditions, in which they are never in contact with any microorganisms and carry no microbiome in their guts.
They observed that the antibiotic treatment exacerbated ALS symptoms. Specifically, researchers tested the animals’ motor performance using different tests — rotarod locomotor test and the hanging-wire grip test — and saw that the animals without a microbiome performed significantly worse. Also, further analyses of the animals’ brains showed a decrease in the number of motor neurons, shrinkage of the brain, and neurodegeneration.
While control (wild-type) mice were able to grow in germ-free conditions, the ALS mice kept dying. Overall, these findings suggested a link between microbiome alterations and ALS disease progression.
Researchers then compared the microbiome composition of ALS mice with that of healthy mice using advanced computational models. The results showed that the microbial composition of the ALS mice was different from the healthy animals, and suggested 11 microorganisms that could play a role in the severity of ALS progression.
To test their roles, they provided the 11 strains, one by one as oral supplements, to ALS mice that were treated with antibiotics.
“One strain significantly slowed disease progression in the mice and prolonged their survival,” researchers wrote. The specific bacteria strain is called Akkermansia muciniphila. In fact, the abundance of this particular bacteria reduced gradually as disease progressed in the ALS mice.
Meanwhile, two other bacteria — Ruminococcus torques and Parabacteroides distasonis — worsened ALS symptoms.
In order to understand the protective role of Akkermansia muciniphila, researchers looked at its metabolites (the products of the bacteria functioning) and identified nicotinamide. The bacteria-produced nicotinamide was found in the blood and cerebrospinal fluid (the liquid bathing the brain and spinal cord) after giving the bacteria to ALS mice. Nicotinamide levels decreased after treatment with antibiotics.
To validate that nicotinamide was indeed responsible for symptoms’ improvement, the team administered this substance continuously to ALS mice and saw that the animals improved significantly. A genetic analysis revealed that nicotinamide benefits may be linked with improvements in mitochondria function, the nerve cells’ powerhouses.
To find out whether these findings could be applied to human subjects, they then analyzed the metabolic and microbiome profile of 37 ALS patients, together with 29 aged-matched healthy family members living in the same household. (They’re expected to have similar microbiomes.)
Genetic analysis of the stools of ALS patients showed that their microbiome composition was significantly different from their healthy relatives. Researchers also saw that genes involved in nicotinamide production were less active in the ALS patients’ microbiome.
When they looked at metabolites in ALS patients’ blood, they found that nicotinamide and its intermediary molecules were significantly reduced. Moreover, nicotinamide levels were decreased in the brains of 60 ALS patients compared to controls; this reduction was associated with enhanced muscle weakness.
“Our long-standing scientific and medical goal is to elucidate the impact of the microbiome on human health and disease, with the brain being a fascinating new frontier,” said Eran Elinav, MD, PhD, Weizmann Institute of Science professor and co-lead author of the study.
While “these findings are only a first step towards achieving a comprehensive understanding of the potential impact of the microbiome on ALS,” Elinav said, “they suggest that in the future, various means of altering the microbiome may be harnessed for developing new therapeutic options for ALS.”