Gene Silencing Method Shows Promise to Treat Familial ALS Associated With SOD1 Mutations
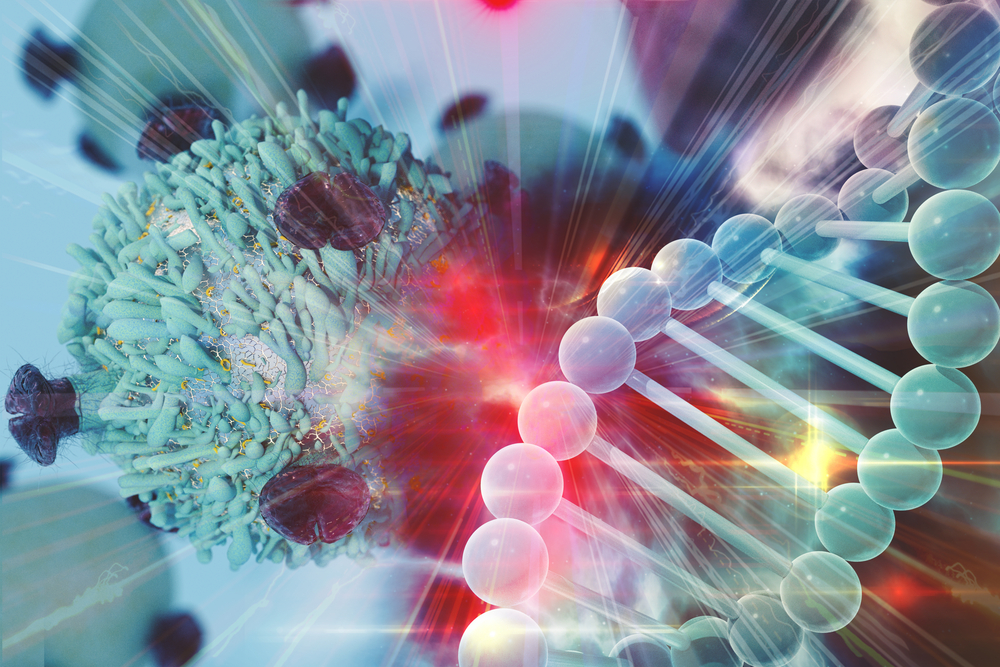
A single dose of an artificial microRNA — a tiny RNA molecule that is able to control the activity of certain genes — can lower the activity of SOD1, a gene commonly mutated in patients with familial amyotrophic lateral sclerosis (ALS), a proof-of-concept study shows.
According to researchers, these early findings suggest the new form of gene silencing (inactivation) may be used as a therapy for familial ALS patients carrying mutations in the SOD1 gene.
The study, “SOD1 Suppression with Adeno-Associated Virus and MicroRNA in Familial ALS,” was published in The New England Journal of Medicine.
Familial ALS is an inherited form of the disease that accounts for up to 10% of all cases of ALS and can be caused by genetic mutations in several genes, including SOD1, which provides instructions to make an enzyme called superoxide dismutase.
This enzyme normally is responsible for destroying toxic substances resulting from a cell’s normal metabolism (reactive oxygen species, or ROS). However, when SOD1 is mutated, the enzyme starts to malfunction, leading to the onset of ALS.
Researchers at the University of Massachusetts Medical School (UMMS) and their colleagues reported the findings of a proof-of-concept study that sought to assess the feasibility of a new method of gene silencing that could be used to shut down the activity of mutated SOD1 in patients with familial ALS.
They used a harmless adeno-associated virus (AAV) to deliver a man-made microRNA specifically designed to prevent RNA molecules produced from the mutated SOD1 gene — called messenger RNA (mRNA) — from being used by cells as a template to make a dysfunctional superoxide dismutase.
“A theoretical advantage of viral vector-mediated gene suppression is the potential for the sustained effect of a single dose of therapy, which is balanced by the possibility that viral vectors may mediate long-lasting adverse effects,” the researchers wrote.
The artificial microRNA was made in a way to recognize a portion of the SOD1 mRNA sequence that can be found in almost all SOD1 mutations, to maximize the number of patients for whom this method could work.
“Otherwise, each unique mutation sequence would require its own drug to silence,” Christian Mueller, PhD, associate professor of pediatrics and first author of the study, said in a UMMS news story.
“This approach allows us to target the vast majority of the patients with an SOD1 mutation using a single drug,” Mueller said.
During the study, two ALS patients, two men ages 22 and 56, received a single infusion of a solution containing the man-made microRNA that was delivered directly to their spinal canal (intrathecal delivery).
The younger patient (patient 1) died of respiratory arrest 15.6 months after beginning treatment and 20.5 months after the onset of ALS symptoms.
In that patient, the levels of superoxide dismutase found in tissues (analyzed post-mortem) along the entire length of the spinal cord were lower than those seen in untreated patients carrying mutations in SOD1 and in healthy individuals, suggesting the virus successfully delivered the microRNA to cells. However, the therapy did not seem to have an effect on superoxide dismutase levels in the cerebral spinal fluid (CSF, the liquid that surrounds the brain and spinal cord).
“The biggest takeaway from this study is that we delivered a new class of silencing gene therapy to patients and suppressed levels of the ALS gene SOD1 quite effectively,” Mueller said.
Patient 1 experienced a temporary improvement in muscle strength in his right leg, but no improvements in lung function. The older patient (patient 2) remained stable over the course of one year.
The first patient had an inflammation of the spinal cord triggered by an immune reaction against the viral vector following infusion, which was avoided by giving the second patient immunosuppressants prior to treatment.
“In the current study there appears to be silencing of the SOD1 gene and a suggestion of clinical benefit. Equally important, we learned how to manage the potential side effects of the drug through immunosuppression,” said Robert H. Brown Jr., MD, PhD, professor of neurology and director of the Program in Neurotherapeutics at UMMS, and senior author of the study.
“The next step for the program will be to test the clinical efficacy of the second generation of this clinical candidate in a placebo controlled trial,” Mueller said.