Protein Related to ALS Onset Used to Develop New Method of Antibody Validation for Use in Research
Scientists have developed a new method to validate antibodies for research, demonstrating its effectiveness by using the protein encoded by the C9ORF72 gene, which, when mutated, may cause amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD), a study reports.
They also urged its implementation in labs around the world to avoid data inconsistency and lack of reproducibility in scientific research.
The study, “Implementation of an antibody characterization procedure and application to the major ALS/FTD disease gene C9ORF72,” was published in the journal eLife.
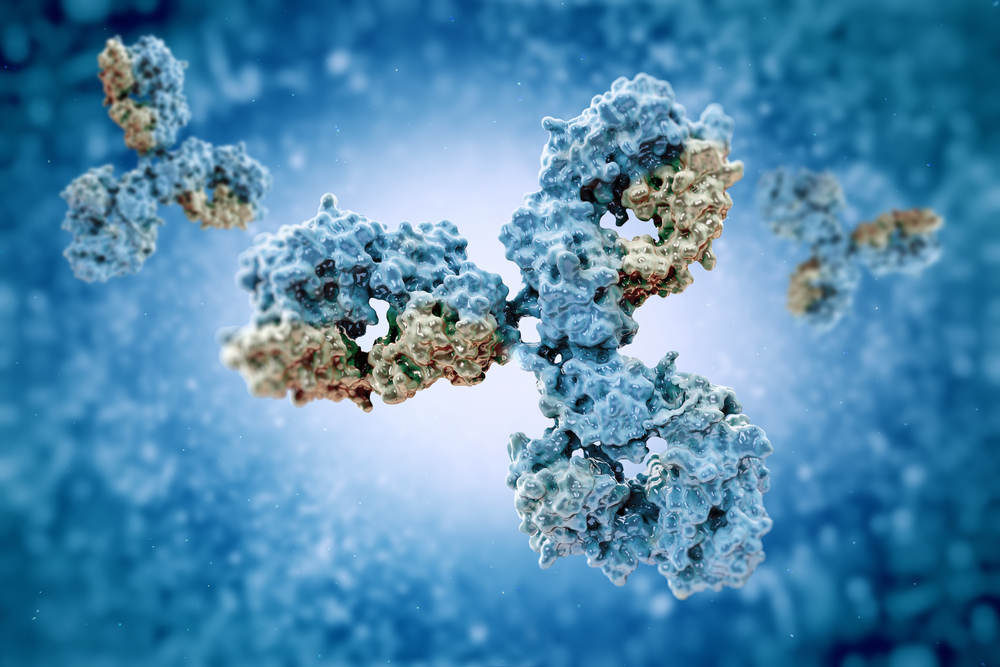
Antibodies are molecules designed to recognize specific regions of a protein. They serve many different purposes in biomedical research, including allowing investigators to study protein localization within a tissue or cell, as well as to measure its levels.
“Antibodies are vital tools in the biomedical research arsenal and in keeping with their importance there are over a million unique antibodies that are commercially available,” the researchers wrote.
However, little attention has been paid to antibody characterization or to the implementation of standardized procedures to ensure the quality of this process.
“As a result, most products are generated and then sold/distributed with only rudimentary and non-quantitative supporting data, and as a result there are serious flaws in the reliability of many of the available reagents,” the authors wrote.
This has raised concerns among the scientific community regarding the validity of findings reported in studies using non-validated commercial antibodies, and called for the development and implementation of a new method that would allow investigators to assess the quality of a specific antibody of interest before using it in their experiments.
In this study, researchers at The Neuro (Montreal Neurological Institute and Hospital) and collaborators described a new method to validate antibodies, using the protein encoded by the C9ORF72 gene as a test case.
“C9ORF72 provides an excellent protein on which to develop an antibody characterization process because although the protein is of relatively low abundance, there are many commercially-available antibodies,” they said. “The process we outline can be applied to any protein target and here it led us to the recognition of problems with the C9ORF72 literature.”
After testing 16 commercial antibodies marketed as being specific for C9ORF72, the team discovered that only one of these antibodies was able to detect the C9ORF72 protein in immunofluorescence, a technique that allows researchers to see under a microscope where in a cell or a tissue a protein labeled by a specific antibody is present.
In other tests, the team found that only two other antibodies seemed to specifically recognize the C9ORF72 protein.
In addition, after examining the literature, they found that none of the antibodies that passed their tests had been used in any study, while several of those that failed to meet their validation criteria had been used in many studies.
These findings question the validity of observations made in previous studies that used antibodies that were either unable to recognize the C9ORF72 protein altogether or detected additional unspecific protein. They also highlighted the importance of establishing a standardized antibody validation protocol that can be adopted by labs worldwide.
“As we worked on our C9ORF72 paper, it became less about one gene and more about a template other labs can use to validate antibodies,” Peter McPherson, PhD, corresponding author of the study, said in a press release.
“The procedures we use are not revolutionary, and in fact this makes our approach widely applicable to any laboratory skilled in the art, yet to my knowledge this is one of the first papers to describe a streamlined process for antibody validation. A large part of the reproducibility crisis is because of poor antibody validation. We owe it to funders and patients to do better,” added McPherson, who is a professor of neurology and neurosurgery and anatomy and cell biology at The Neuro.