Mouse Study Uncovers Role of FUS Protein in ALS Neuromuscular Junction Defects
FUS protein plays a role in the proper functioning and stability of the neuromuscular junction — the site of communication between motor nerves and muscle fibers — and mutations in this protein appear to be toxic to both motor neurons and muscle cells, causing features of amyotrophic lateral sclerosis (ALS), a study has found.
While it has been known for a long time that the neuromuscular junction (NMJ) is abnormal in ALS, “this is the first time that a gene associated with ALS has been directly implicated in NMJ maintenance and stability,” researchers wrote in the study.
The study, “FUS-mediated regulation of acetylcholine receptor transcription at neuromuscular junctions is compromised in amyotrophic lateral sclerosis,” was published in the journal Nature Neuroscience.
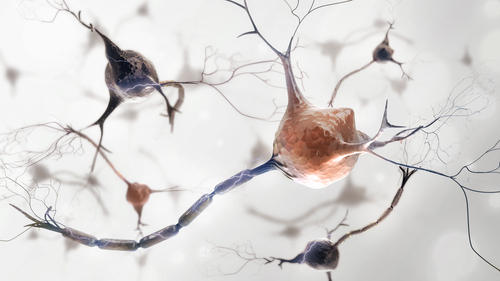
The neuromuscular junction (NMJ) is the place where motor neurons make contact with muscle cells. When the neuron releases certain neurotransmitters (predominantly acetylcholine), they bind to receptors on the muscle cell in a region called the endplate, which ultimately signals the muscle cell to contract or not.
Problems with the NMJ have been implicated in a number of diseases, including ALS, but the mechanisms behind this association remain poorly understood. In the new study, researchers examined NMJs in mouse models of ALS in order to better understand this connection.
Specifically, researchers looked at mice that either had mutations in the FUS gene, or lacked the gene entirely. FUS, which provides instructions to make a protein of the same name, is mutated in about 5% of familial ALS cases and about 1% of sporadic cases.
The researchers first found that the size of muscle endplates was reduced by about 17% in FUS-mutant mice, though endplate size was unaffected in mice that completely lacked FUS. Both mice, however, had fewer total endplates — decreases of about 33% and 44%, respectively.
That finding may seem paradoxical, but it makes sense in the context of the particular type of mutation in FUS. The FUS protein normally gets transported into the nucleus — the part of the cell that contains DNA — where it has important roles in regulating gene transcription (that is, turning genes on and off).
In order to get into the nucleus, the FUS protein has a signal sequence — a sort of code that tells the cell, “this protein goes into the nucleus.” The mutant FUS (both in the mice and in humans with ALS), however, doesn’t have these signals, so it just stays in the cell’s cytoplasm. The researchers found that having this protein in the cytoplasm was toxic to muscle cells, even more so than the toxicity that already would be present if there were no FUS protein at all.
The researchers then looked in more detail at the role FUS normally plays in the nuclei of muscle cells. Muscle cells, unlike most other kinds of cells, have multiple nuclei, and the nuclei that are right below endplates “turn on” a specific set of genes called Chrn genes, which originate the acetylcholine receptor.
The researchers found that muscle nuclei that didn’t have FUS were impaired in their ability to “turn on” these genes, essentially being unable to perceive signals from nerve cells. This process also was dependent on another protein, called ERM (also known as ETV5), which has a well-established role in “turning on” Chrn genes. The researchers demonstrated that ERM and FUS physically interact with each other, cooperating in order to carry out this important function.
“[W]e discovered that FUS and ERM collaborate to promote the transcription of Chrn genes in subsynaptic [muscle] nuclei,” the researchers wrote in summation of these findings.
The researchers validated many of these findings in cells from people with ALS — both muscle cells, taken directly from biopsies, and cells grown from patient-derived stem cells. For instance, they found evidence of reduced endplate area and impaired transcription of Chrn genes in these cells.
These findings are particularly noteworthy because, broadly, ALS is considered a disease of motor neurons, not the muscles themselves. The study results suggest, however, that FUS plays an important role in muscle cells that has been unrecognized so far and may be important in the pathology of ALS.
“Impairment of this novel FUS function in FUS-ALS [ALS caused by mutant FUS] mouse and cell models suggests that, possibly, the intrinsic toxicity of mutant FUS in skeletal muscle may contribute to the dying-back motor neuronopathy in patients with FUS-ALS,” the researchers concluded.






