Poorer Ability to Regulate Body Temperature May Be ALS Symptom, Mouse Study Suggests
Written by |
A diminished ability to regulate body temperature may be a manifestation of amyotrophic lateral sclerosis (ALS), results of a mice study suggest.
Such a diminishment could be related to problems in controlling the naturally occurring circadian clocks that regulate tissues and organs. The circadian rhythm is an important mechanism that works as an auto-management system, indicating to organs when it is day or night, when they should be more active or less.
The study, “Defective daily temperature regulation in a mouse model of amyotrophic lateral sclerosis,” was published at the journal Experimental Neurology.
Previous studies have demonstrated that mice in ALS disease models show higher-than-usual energy expenditure and have a lower body weight when compared to healthy animals.
While lower food consumption is one plausible explanation for this odd combination, the researchers failed to find any changes in food intake and exercise when comparing the two group of animals.
Mice in a laboratory spend most of their energy working to manage their body temperature. Alterations in these processes could, in part, explain the reported increase in energy expenditure and reduced body weight.
A team led by researchers at the University of Massachusetts Medical School designed a study to better understand body temperature regulation and ALS.
They used mice genetically engineered to carry the mutated version of the human SOD1 gene known to cause familial ALS, and compared findings with healthy mice.
Small sensors that recorded body temperature every 15 minutes were surgically placed in mice’s abdominal cavity, in a way that did not interfere with the animals’ normal activity.
Results showed that, in both groups, the animals had higher temperature during the night (when they are active) and lower body temperature during the day (when they are resting), a is normal body temperature pattern.
However, mice with the mutated SOD1 gene were found to have a lower body temperature during the night compared to healthy mice. In fact, the overall 24-hour swing in body temperature between day and night activities was lesser in the ALS animals.
This difference between the two mouse groups became progressively more marked as they aged (older than 100 days). Day-to-night (light-to-dark) body temperature changes (the 24-hour cycle) became smaller and shorter as ALS mice got older, whereas they remained stable in healthy control mice it remained stable.
Interestingly, the researchers found this diminished ability to regulate body temperature became more marked as the animals started to show ALS symptoms, as determined by significant differences in grip strength. This suggests that, although the mechanisms regulating temperature were most likely impaired before symptoms were evident, additional difficulties might be due, at least in part, to inadequate heat production by tissues affected by the disease as it progresses.
As with earlier studies, no changes in locomotor activity or eating behaviors were evident between the groups that might explain or contribute to the poorer regulation of body temperature observed.
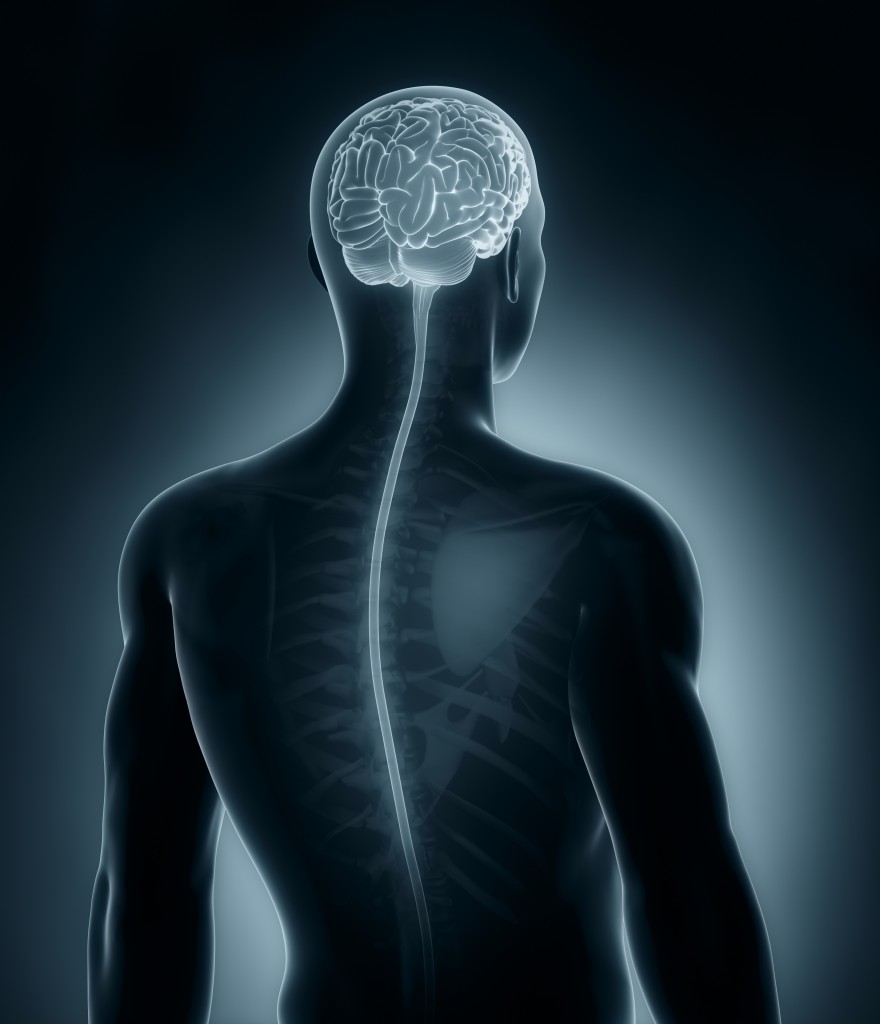
An analysis of the mice’s brain found the human SOD1 gene to be present, including in areas linked to body thermoregulation such as the hypothalamus.
Based on these findings, the team believes that the ALS-related “dysregulated daily body temperature rhythm” could start an0 impaired “central” mechanism, “perhaps involving specific neural output pathways” in the hypothalamus. Later, these problems are compounded by an added a “peripheral” impaired process, “as thermogenic [heat producing] organs progressively fail.”
Recent studies in ALS patients have shown that defects in the hypothalamus could be implicated in disease development and progression. In particular, brain imaging studies show evidence of atrophy in the anterior hypothalamic region being present in ALS, which could be related to dysregulated body temperature in these patients.