Certain Blood Markers Linked to Different Stages of ALS, Study Suggests
Written by |
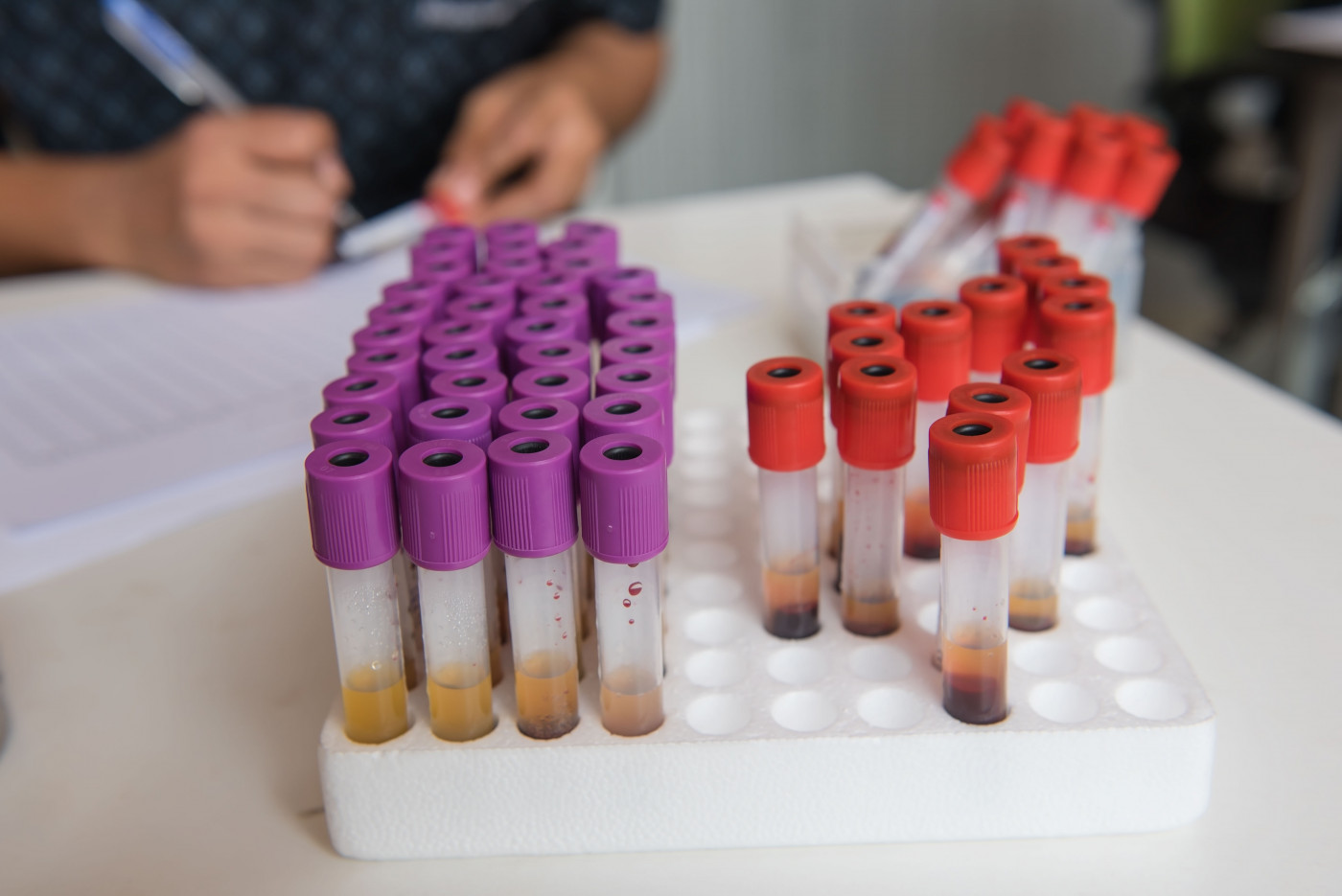
Differences in blood parameters, such as total protein levels, are associated with different stages of amyotrophic lateral sclerosis (ALS), meaning they could become valuable biomarkers to track disease progression in clinical practice, a study suggests.
The study, “Clinical disease stage related changes of serological factors in amyotrophic lateral sclerosis,” was published in the journal Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration.
Blood work is a routine part of healthcare, and ALS is no exception. Previous studies have shown there are differences in the levels of various molecules in the blood between people with and without ALS, yet these studies generally hadn’t examined whether there were differences among ALS patients in different stages of the disease.
To address this lack of knowledge, researchers recruited 571 ALS patients at their hospital in China, as well as 571 individuals used as controls who were matched for factors including age and sex. Slightly more than half of the patients were males, and just under a quarter had the bulbar form, which is just slightly lower than what would be expected.
Discuss the latest research in the ALS News Today forums!
The researchers divided ALS patients into stages using the King’s College staging system, which categorizes patients into four stages based on disease severity, from stage 1 (the least severe, with the initial onset of symptoms) to stage 4 (most severe, requiring intervention such as ventilation). In the recruited group, there were 106 stage 1 patients, 240 stage 2 patients, 131 stage 3 patients, and 37 stage 4 patients.
The investigators compared the levels of various molecules in the blood between ALS patients and controls and between patients at different stages of ALS.
Most notably, the researchers found that uric acid (an antioxidant), albumin (a protein made by the liver), and total protein levels were lower in ALS patients. Furthermore, lower levels of these markers were correlated with higher stages; that is, stage 4 ALS patients had, on average, the lowest levels of all three of these markers.
Other blood contents, such as cholesterol, also varied between ALS patients and controls. However, none of these markers correlated with disease stage — or, at least, there wasn’t a statistically significant association. This means that, although some trends were noticed, it wasn’t possible for the researchers to rule out the possibility that these trends were just chance.
Additionally, some of the detected correlations only seemed to apply to certain groups of patients. For example, while lower total protein levels correlated with higher disease stage among all patients, when the investigators divided the ALS patients by sex, this correlation remained for male ALS patients, but not females.
This study is a step toward using blood tests to more accurately predict the prognoses of ALS patients. Future studies might give a clearer picture of just how these differences can be used in the clinic, and larger studies with more patients might make it clearer whether trends that didn’t reach statistical significance in this study are reflective of actual changes or just chance.
Additionally, the fact that there are any measurable physiological changes that correlate with staging suggests that the King’s College staging system — which is less than a decade old— is actually reflecting changes in what’s going on in the body that might be driving the progression of the disease, not just the symptoms and signs that are outcomes.
“The association of these serological values with disease stage suggests that the staging system can be used to evaluate the disease burden and disease progression in ALS, and these metabolite based candidates would be linked to ALS pathogenesis [disease progression] and may have clinical utility in clinical practice,” the researchers concluded.