Inhibiting cellular stress response may help with rare ALS type: Study
Possible therapeutic target normalizes processes, function in motor neurons
Written by |
For a rare type of amyotrophic lateral sclerosis (ALS), inhibiting a cellular stress response can normalize processes and function in specialized nerve cells called motor neurons, suggesting this response is a possible therapeutic target, a study reports.
These results are specific to ALS related to the P56S mutation in the VAPB gene, a rare genetic abnormality more commonly found in Brazil. However, the findings may have broader applicability in ALS and suggest the importance of considering genetic makeup in clinical trials, according to lead researcher Helen Cristina Miranda, PhD, of Case Western Reserve University.
“This work could help lay the foundation for genetically informed clinical trials,” Miranda said in a university news story.
Miranda’s team also investigated the molecular pathways by which P56S mutations lead to disease processes. They identified a disruption in how parts of cells bind to each other, which could help explain motor neuron changes in ALS.
The study, “Convergent activation of the integrated stress response and ER–mitochondria uncoupling in VAPB-associated ALS,” was published in the journal EMBO Molecular Medicine.
Mechanisms behind ALS-causing mutations explored
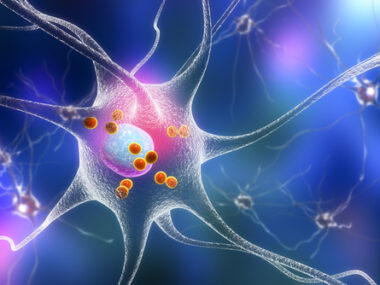
In ALS, the motor neurons that control voluntary movement progressively die, leading to muscle weakness and other symptoms. Genetics is a possible cause, with mutations in several genes linked to ALS development.
However, “despite decades of research, the mechanisms by which specific ALS-causing mutations lead to neurodegeneration remain poorly defined, limiting therapeutic advances,” the researchers wrote.
As with other genetic mutations, researchers don’t yet understand the mechanisms by which P56S mutations in VAPB lead to ALS. Specifically, these mutations cause a familial form of ALS called ALS type 8, or ALS8.
VAPB contains instructions for cells to manufacture a protein of the same name. The VAPB protein helps tether the endoplasmic reticulum (ER), a structure within cells, to other proteins and structures. The ER is essential for proper cellular function and helps ensure proteins fold correctly.
Disruptions in VAPB impair the protein’s role in linking the ER to mitochondria, another cellular structure that helps generate energy.
These links are “especially important in nerve cells,” Miranda said. “When they break down, the neurons become more vulnerable to degeneration.”
Disrupting ER MAM can contribute to cellular stress
To investigate the relationship between mutated VAPB and neuronal dysfunction, the team used motor neurons derived from induced pluripotent stem cells (iPSCs), which can develop into multiple types of cells. They genetically engineered some of the cells to have P56S mutations.
Compared to healthy motor neurons, mutated ones showed less activity. The researchers traced this to problems with VAPB’s ability to tether the mitochondria to the ER. This disrupted the points of contact between these structures, called the ER mitochondrial-associated membrane (ER MAM).
Disrupting the ER MAM can contribute to cellular stress and activate a cell’s integrated stress response (ISR). This is what the team saw in the motor neurons — sensitivity to stress was higher and adaptation to it was impaired in mutated cells relative to healthy ones. The ISR can initially be helpful by enabling a cell to adapt to a diverse stimuli and changes in gene activity. Over time, however, it may lead to cell damage.
“This is the first study to mechanistically connect a known ALS mutation with ISR activation, highlighting the potential for mutation-specific therapeutic targeting and patient stratification in ISR-modulating clinical trials,” the researchers wrote.
ISR inhibition, an approach used to assess whether the ISR was responsible for the observed functional changes in cells, normalized protein production and neuronal firing, which were dysfunctional in the mutated cells. Neuronal firing refers to electric impulses through which nerve cells communicate.
We also showed that blocking this stress response can reverse damage in the lab. That’s a promising proof-of-concept for future therapeutic strategies.
For validation, the researchers also looked at motor neurons derived from iPSCs from individuals with P56S-related ALS. As with the engineered neurons, they demonstrated consistent problems with the ER MAM and ISR activation.
“We also showed that blocking this stress response can reverse damage in the lab,” Miranda said. “That’s a promising proof-of-concept for future therapeutic strategies.”
Previous clinical trials have tested targeting the ISR as a strategy for treating ALS. However, their primary efficacy goals were not met.
“These outcomes underscore the urgent need for mechanistic insight into how and when ISR modulation may benefit ALS patients,” the team wrote.
While the P56S mutation is very rare, “studying it gives us a window into how ALS motor neurons respond to stress,” Miranda said. “We are now testing ISR inhibitors in more complex neuromuscular models and exploring how this approach might benefit other ALS subtypes.”