Mitochondria Play a Critical Role in Neuroinflammation, Neuron Cell Death, Study Reveals
Written by |
The release of fragmented or dysfunctional mitochondria — a cell’s powerhouse — by immune and structural cells inside the central nervous system is a critical step that triggers neuron death and the progression of human neurodegenerative diseases such as amyotrophic lateral sclerosis (ALS), a study shows.
Led by researchers at the Stanford University School of Medicine, the study demonstrates that targeted inhibition of mitochondria fission may represent a new strategy for preventing nerve cell death across such disorders as ALS, Alzheimer’s disease, and Huntington’s disease.
This finding was reported in “Fragmented mitochondria released from microglia trigger A1 astrocytic response and propagate inflammatory neurodegeneration,” a study published in the journal Nature Neuroscience.
About seven years ago, a Stanford chemical and systems biology professor and her colleagues designed a small protein — which they called P110 — that had the ability to specifically block signals that could induce the fragmentation of mitochondria.
Now, the team led by Daria Mochly-Rosen, PhD, the senior author of the study, took a closer look at the impact of this protein on the nerve cells of the central nervous system.
The ALS News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
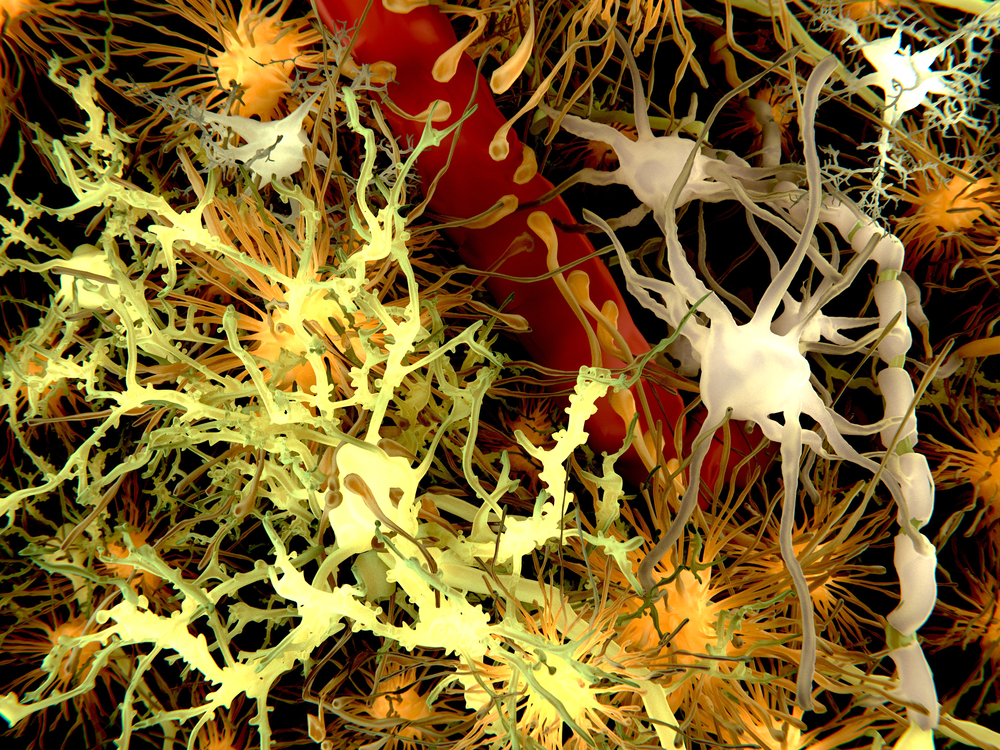
The scientists started by treating mice that had Alzheimer’s, Huntington’s, and ALS with P110 or a placebo, and collecting brain tissue samples for analysis. They found that mice that received placebo showed signs of activation of both microglia, or immune cells, and astrocytes, which are structural and supportive cells. Meanwhile, the mice treated with P110 showed evidence of less cell activation and slower disease progression.
Treatment with P110 also significantly reduced the amount of amyloid-beta aggregates, or clumps, which are linked with several neurological diseases. The protein also improved mitochondrial health and reduced neuroinflammation. The research showed P110 expanded the mice’s lifespans.
Next, the team cultured microglia cells in the lab. The scientists found that these cells released mitochondria and active signaling molecules into their surroundings when they were exposed to stressful stimulus, such as disease-related toxic protein aggregates. If astrocytes were cultured into this broth, the cells would become activated, suggesting a direct transfer of pro-inflammatory signals between microglia and astrocytes.
Additional detailed experiments revealed that the positive effects of P110 were mostly supported by preventing the release of damaged or fragmented mitochondria by microglia cells into the brain tissue milieu and consequent activation of astrocytes.
“Most people have thought that mitochondria situated outside of cells must be ghosts of dead or dying cells,” Mochly-Rosen said in a press release written by Bruce Goldman. “But we found plenty of high-functioning mitochondria in the culture broth, along with damaged ones. And the glial cells releasing them appear very much alive.”
The researchers note that even healthy cells routinely release mitochondria into their surrounding environment.
“Clinical and experimental studies have identified fragmented mitochondria in biofluids of patients afflicted by subarachnoid hemorrhage and of patients affected by stroke, which suggests that their presence in the extracellular space is a biomarker for neurodegeneration and disease severity,” the researchers said.
Indeed, the higher the amount of dysfunctional or fragmented mitochondria was in the surrounding tissue, the higher were the levels of neuroinflammation and neuron death.
The process of disease-related mitochondria fission was found to be mediated by the Drp1-Fis1 signaling pathway, which was blocked by P110. In contrast, treatment with P110 had no effect on another similar signaling pathway mediated by Drp1 and Mff proteins that is necessary for physiological mitochondria fission, which is required to maintain mitochondria health.
This selective effect also may represent a positive therapeutic feature of P110. The protein may support the transfer of more healthy mitochondrial into the neurons milieu while preventing the deleterious effects of disease-associated mitochondrial fission.
The team is still working to better understand how released damaged mitochondria can induce inflammation and neuronal cell death.
Mochly-Rosen and postdoctoral scholar Amit Joshi, PhD, the lead author of the study, have filed for a patent on P110 and its utility in Huntington’s disease, ALS, and other neurodegenerative diseases.