Researchers Probe Neurofilaments’ Potential as Biomarkers for ALS Progression
Written by |
An analysis of previously published data suggests that neurofilaments in the blood and spinal fluid of people with amyotrophic lateral sclerosis (ALS) may be used to assess disease progression and neurodegeneration in general.
Levels of the factor also were higher in ALS patients than in patients with diseases mimicking ALS, suggesting that neurofilament also might be explored to aid diagnosis. According to the researchers, however, this scenario is less likely because neurofilament also is present in other neurological conditions.
The study, “Neurofilaments as Biomarkers for Amyotrophic Lateral Sclerosis: A Systematic Review and Meta-Analysis,” was published in the journal PLOS ONE.
Neurofilament is a component of nerve cells, and as those cells die, the factor can be found in the bloodstream or cerebrospinal fluid of patients. Numerous studies have investigated neurofilament in ALS, but have not always reached the same conclusion.
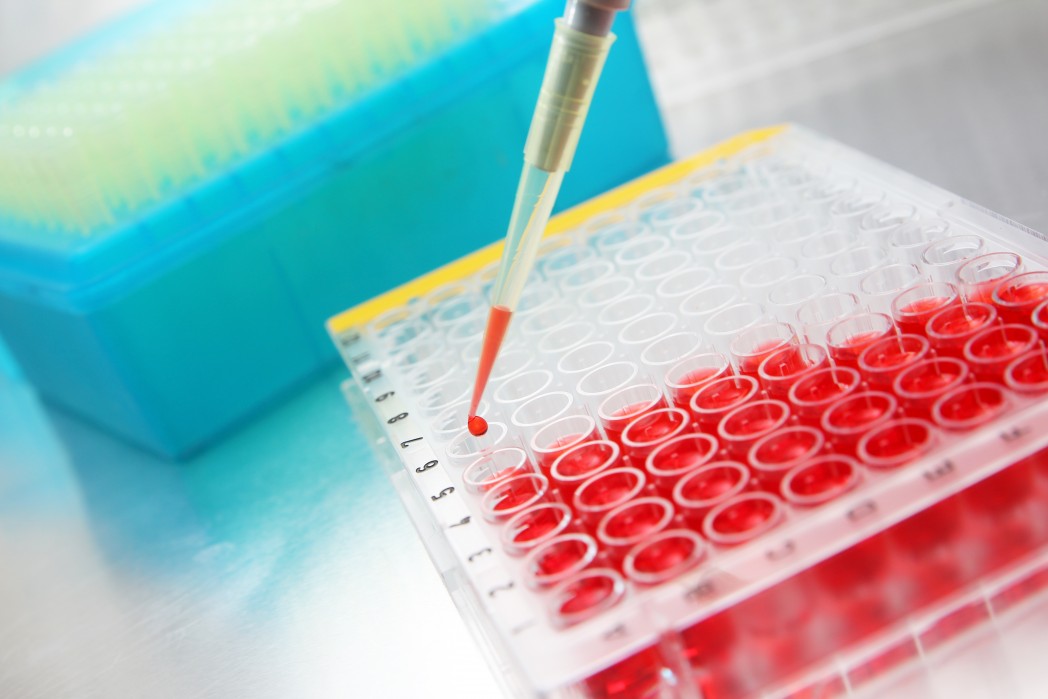
To get a clearer picture, researchers from the University of Queensland in Australia analyzed previously published studies on the topic. Of 49 studies found, only 15 held enough information to allow researchers to include them in the analysis.
Neurofilament exists in three different forms; heavy, intermediate and light. The analysis focused on heavy and light forms.
The research team found that heavy neurofilament was higher in the cerebrospinal fluid of ALS patients than in healthy people or people with diseases resembling ALS. Compared to people with other neurological diseases, there was, however, no difference.
The factor also was not higher in the blood of ALS patients than in healthy people, or those with diseases not impacting the brain or spinal cord.
The light variant of neurofilament was higher in the spinal fluid of ALS patients than in control subjects, people with ALS mimic disease, and people with other types of neurological disease.
The team also found that both forms of neurofilaments were linked to disease duration, and the heavy variant was associated with ALSFRS-R score — an estimate of a patient’s impairment, which can be used to assess response to treatment or progression of the disease.
Since the various studies used different types of statistical methods to analyze results, it was impossible to analyze the correlation between neurofilament levels and survival. Several studies, however, pointed out that higher levels of neurofilament were linked to shorter survival times.
Ultimately, the team concluded that if neurofilament is to be used as a biomarker, more studies are needed and methods need to be standardized to make comparisons between studies possible.