Experimental Test Could Detect ALS Before Symptom Onset
A method that measures tiny amounts of aggregated TDP-43 protein in the cerebrospinal fluid may have the potential to detect amyotrophic lateral sclerosis (ALS) in the early stages of the disease, potentially before symptom onset, a study reports.
The study, “TDP-43 real-time quaking induced conversion reaction optimization and detection of seeding activity in CSF of amyotrophic lateral sclerosis and frontotemporal dementia patients,” was published in the journal Brain Communications.
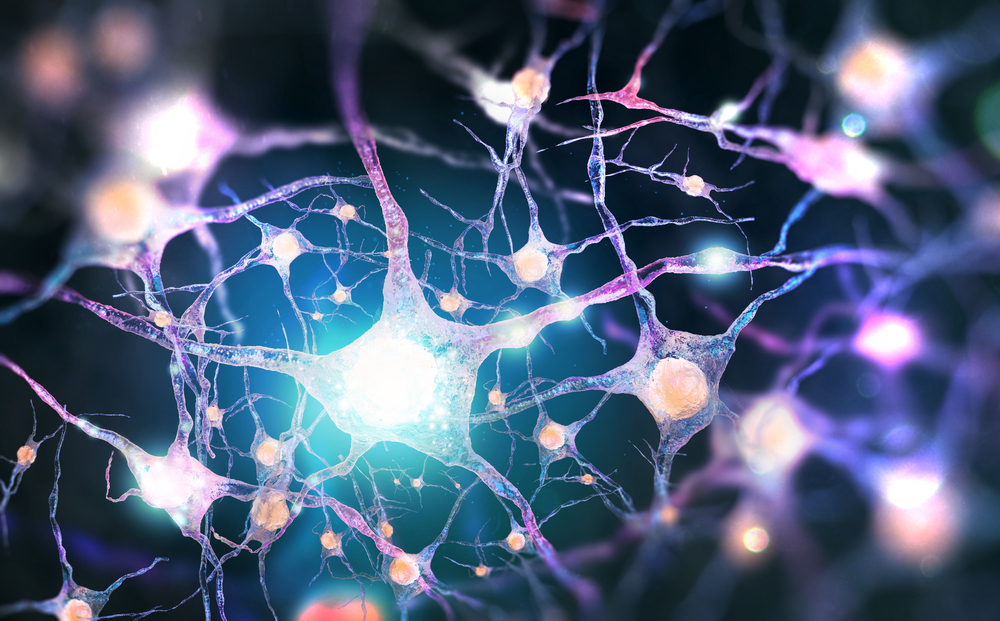
The toxic buildup of the transactive response DNA-binding protein-43, or TDP-43, occurs in about 97% of people with ALS, and roughly 45% of people with a similar condition with genetic and clinical overlap called frontotemporal dementia (FTD).
Because ALS is usually diagnosed at least a year after symptoms begin, once the disease is well established, methods to detect TDP-43 buildup may help identify those in the early stages, before symptoms appear. This would allow a larger therapeutic window and serve as a marker for disease progression and the effects of treatments.
Studies have suggested that aggregates of TDP-43 form like a prion — a misfolded protein, called a “seed,” that triggers the conversion of normal protein into a misfolded, abnormal form, which, in turn, converts more protein, causing the buildup of aggregates.
However, detecting TDP-43 prions is challenging due to the very small quantities available for testing, especially in the condition’s early stages.
A technique known as real-time quaking-induced conversion reaction (RT-QuIC) has been developed to amplify and detect small quantities of prions. It has been used to measure prions in people with Alzheimer’s disease and Parkinson’s disease, both characterized by misfolded protein buildup.
Now, investigators at the International School of Advanced Studies (SISSA) in Italy, in collaboration with researchers at facilities across the country, have adapted RT-QuIC to detect TDP-43 prions and tested the method using cerebrospinal fluid (CSF, the fluid surrounding the brain and spinal cord) collected from people with ALS and FTD.
“Many neurodegenerative diseases, such as Alzheimer’s or Parkinson’s, and the diseases caused by prions are characterized by the uncontrolled accumulation of specific proteins in the nerve cells,” Carlo Scialò, PhD, and Giuseppe Legname, PhD, of SISSA, said in a press release. “A test called [RT-QuIC] had already been developed for early identification of the proteins involved in several of these diseases.”
“We thought of using it for the first time for two other diseases, ALS and frontotemporal dementia, where the protein that accumulates is the same: TDP-43,” they added.
To adapt RT-QuIC to measure TDP-43 aggregates, the team first generated a large amount of lab-made human TDP-43 protein (HuTDP-43), then tested different conditions such as protein concentration, temperature, pH, and shaking protocol to find the best conditions for HuTDP-43 aggregation.
Since one part of the TDP-43 protein is known to be more prone to aggregate, a small version with just this portion was also made, named HuTDP-43(263-414). Both forms of HuTDP-43 were analyzed for aggregation properties, and typical prion-like aggregation characteristics were observed.
Using brain homogenates from postmortem patients as seeds, both forms of HuTDP-43 were suitable for following aggregate growth. The smaller form HuTDP-43(263-414) was chosen for further experiments as less was required to achieve the same result.
To validate this method, CSF samples were analyzed from 13 people with ALS and 18 with FTD (21 males, 15 females). To increase the likelihood that CSF contained TDP-43 prion seeds, those selected carried a disease-causing mutation in one of three genes related to TDP-43 pathology: TARDBP, GRN, and C9orf72.
As a comparison, CSF samples from 27 age-matched healthy people (14 males and 13 females), who had undergone a CSF extraction to exclude neurological disease, were also examined and used as controls.
Using HuTDP-43(263-414) as a substrate, CSF from patients efficiently seeded the RT-QuIC reaction in 18 of 19 C9orf72 participants, 13 of 14 GRN samples, and all TARDBP patients. Among controls, four were positive.
Thus, the likelihood of RT-QuIC correctly identifying those with the disease (sensitivity) was 94%, and the ability to correctly find those without the disease (specificity) was 85%.
“The patients involved were all carriers of a particular genetic mutation which we know leads to the accumulation of TDP-43 in the brain,” said Scialò and Legname. “With our system, we identified it in 94% of them, which is an excellent result.”
A final experiment confirmed that, under these experimental conditions, TDP-43 RT-QuIC was not susceptible to the presence of prions associated with Alzheimer’s disease and Parkinson’s disease.
“Our data on TDP-43 RT-QuIC represent a proof-of-concept of its potential for the detection of TDP-43 pathological aggregates,” the investigators wrote in the study. “A further optimization of the presented TDP-43 RT-QuIC protocol would increase the opportunity to perform the earliest and most accurate diagnosis at a single patient level.”