Ozanezumab Fails to Show Benefit as ALS Treatment in Phase 2 Clinical Trial
Written by |

A Phase 2 clinical trial, exploring ozanezumab as a treatment of amyotrophic lateral sclerosis, failed to show any benefits. The data at hand means the search for treatments that may outperform the only approved ALS medication, riluzole, continues.
The study, “Safety and efficacy of ozanezumab in patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled, phase 2 trial,” was led by researchers at Ramsay Generale de Sante Hopital Prive Peupliers in France. The report was published in the journal The Lancet Neurology.
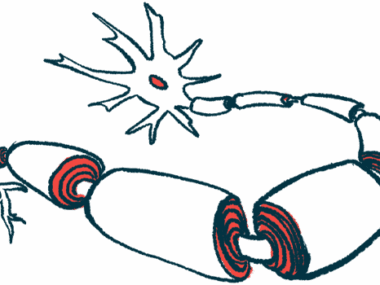
Ozanezumab is an antibody that blocks a protein called Nogo-A (Neurite outgrowth inhibitor A). Studies in a mouse model of the familial form of ALS, caused by mutations in the SOD1 gene, showed that the treatment was beneficial. But as the majority of treatments developed for various diseases, the effects did not translate to a benefit in patients.
The global trial (NCT01753076) was a randomized study, in which ozanezumab was compared to placebo in a double-blind manner. Patients were allowed to continue with riluzole during the study.
In total, 151 patients received placebo, and 152 ozanezumab, which was dosed as a one-hour intravenous infusion every two weeks for 46 weeks. Patients were then assessed at 48 and 60 weeks.
The study’s main outcome was a combination analysis of the ALS Functional Rating Scale-Revised (ALSFRS-R) and overall survival, but at 48 weeks, no differences were reported between treatment and placebo groups in the scores.
In other measures of efficacy, researchers noted that the group receiving ozanezumab had numerically worse outcomes than those in the placebo group on all analyzed outcomes. But these differences were not statistically significant.
Most side effects were common in both groups, except for dyspepsia, depression, and diarrhea that appeared more often among ozanezumab-treated patients. Although four more patients in the ozanezumab group died than in the placebo group, there was no statistical difference in survival rates.
In their report, the research team elaborated on why the drug might have failed, suggesting several possible scenarios. They suggest that the increased levels of Nogo-A, reported in ALS patients, may be a compensatory rather than disease-driving event. They also did not rule out the possibility that targeting Nogo-A may have been harmful to patients.
Ozanezumab, developed by GlaxoSmithKline, was recently tested in a small Phase 1 trial. That study was intended to evaluate the safety of the treatment and not designed to track down efficacy measures, and findings indicated that the drug was safe and may be effective. The current trial dispersed such hopes.
“Ozanezumab did not show efficacy compared with placebo in patients with ALS,” the study concluded. “Therefore, Nogo-A does not seem to be an effective therapeutic target in ALS.”