New Prognosis Model Predicts Risk of Respiratory Insufficiency or Death in ALS Patients, Study Says
Scientists created a new prognosis model to predict the risk of respiratory insufficiency or death within six months of follow-up in patients with amyotrophic lateral sclerosis (ALS).
The study, “Development of a prognostic model of respiratory insufficiency or death in amyotrophic lateral sclerosis,” was published in the European Respiratory Journal.
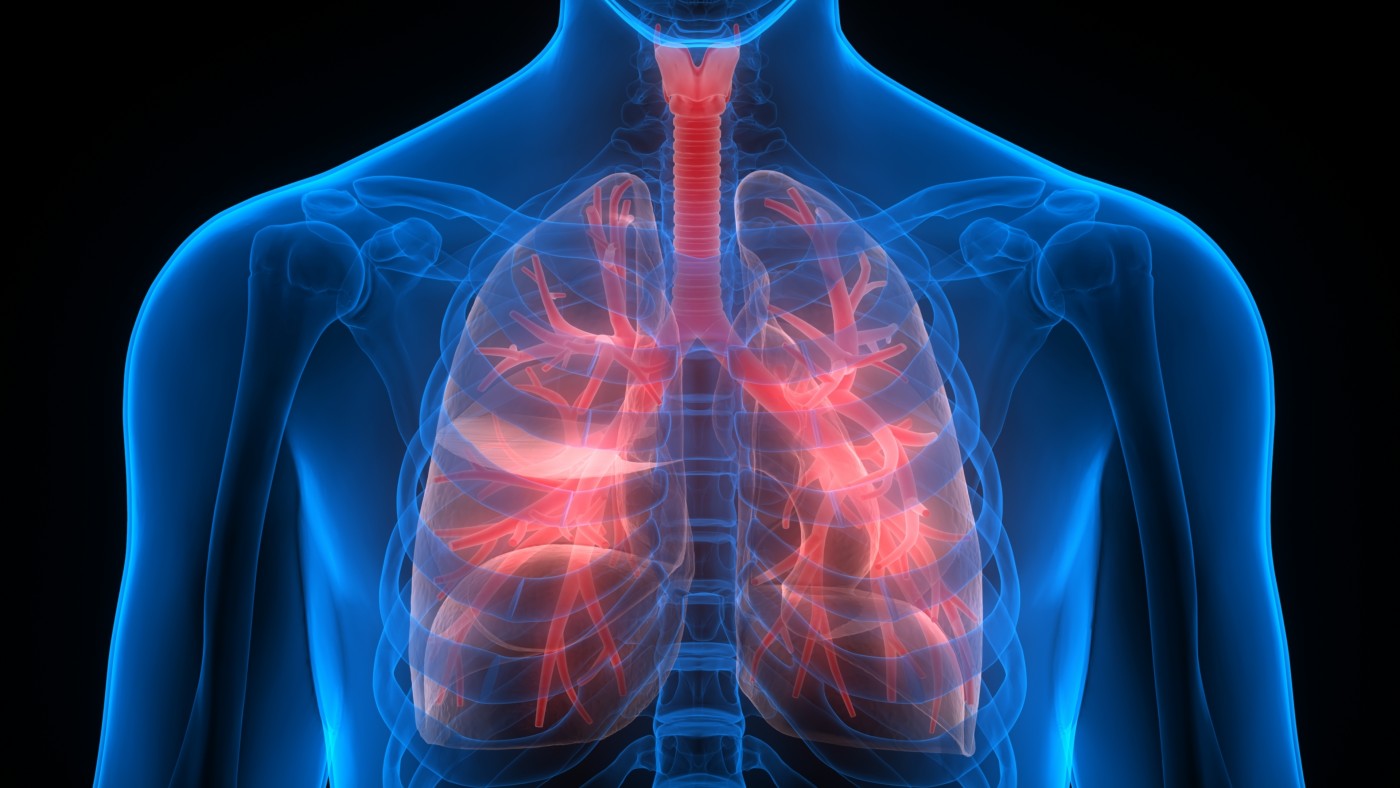
ALS is a progressive neurodegenerative disorder caused by the gradual destruction of motor neurons — nerve cells responsible for voluntary muscle control — in the spinal cord and in the brain.
As the disease worsens, patients eventually lose control of the respiratory muscles, including the diaphragm, which allow the chest to move, causing severe respiratory complications, the most common cause of death for ALS patients.
For this reason, assistive breathing interventions are often recommended for ALS patients, such as noninvasive ventilation, which has been shown to improve quality of life and potentially survival.
However, “shortcomings in current clinical strategies for predicting the onset of respiratory insufficiency have hindered development of practice guidelines and clinical trials,” the researchers wrote.
“Also, the absence of a reliable prognostic model has prevented clinicians from anticipating mechanically-assisted ventilation, thereby limiting the opportunity to prepare patients for shared decision making, improving timeliness of referrals for respiratory interventions, and developing clinical trial design,” they added.
Discuss the latest research in the ALS News Today forums!
In this study, a team of researchers from the Perelman School of Medicine at the University of Pennsylvania set out to develop and validate a new prognosis model that would be able to estimate the onset of respiratory insufficiency in ALS patients who had been closely monitored for six months at an outpatient clinic.
The study included two different groups of ALS patients: 765 patients who were examined between January 2006 and December 2015 at the University of Pennsylvania Comprehensive ALS Center (Penn group); and 7,083 patients whose records had been stored at the Pooled Resource Open-Access ALS Clinical Trials (PRO-ACT) database.
The internal Penn group was used to generate and validate the prognosis model, while the remaining patients’ records were used to validate the model externally. Model predictors included initial (baseline) patient characteristics that were recorded during the first clinic visit.
The study’s primary outcome was to assess the onset of respiratory insufficiency within an observation period of six months. ALS patients were considered to be affected by respiratory insufficiency if they required noninvasive ventilation, had less than 50% of forced vital capacity (the amount of air a patient is able to exhale after taking a deep breath, FVC), underwent a tracheostomy (a surgical procedure in which a hole is drilled in the patients’ windpipe to create an alternate breathing route), or had died.
Results showed that among the 765 patients from the Penn group, 300 (39%) showed signs of respiratory insufficiency or died during the six-month follow-up. Likewise, among the 7,083 patients from the PRO-ACT database, 2,453 (35%) had respiratory insufficiency or died within the same period of time.
A total of six baseline patient characteristics were used as model predictors to estimate the risk of respiratory insufficiency or death, including:
- patients’ age at diagnosis
- delay between the onset of symptoms and disease diagnosis
- FVC
- site of symptom onset
- Amyotrophic lateral sclerosis functional rating scale-revised (ALSFRS-R) total score
- ALSFRS-R dyspnea (shortness of breath) score
“We found that younger age, less diagnostic delay, lower FVC, bulbar symptom onset site, lower ALSFRS-R total, and ALSFRS-R dyspnea lower than 2 at baseline were significantly associated with a higher risk of respiratory insufficiency or death at six months in a large single-center cohort and a dataset of multiple clinical trials in ALS,” the researchers wrote. Bulbar-onset is marked by initial symptoms involving the head and neck, including trouble speaking or swallowing; limb-onset ALS is more common.
After derivation and initial validation, the prognosis model achieved a positive predictive value (the percentage of true positives) of 77%, a negative predictive value (the percentage of true negatives) of 86%, a sensitivity of 83%, and a specificity of 81% for respiratory insufficiency in patients from the Penn group.
External validation of the prognosis model for respiratory insufficiency in patients from the PRO-ACT database led to similar results (positive predictive value of 62%; negative predictive value of 76%; sensitivity of 53%; and specificity of 82%).
“Further studies would be necessary to validate this as a tool prospectively to identify a high-risk subgroup suitable for clinical trial enrollment. In clinical practice, application of the prognostic model may help inform the optimal timing for referral of ALS clinical patients for respiratory care with the goal of delaying (or at least preparing for) the onset of respiratory insufficiency,” the scientists wrote.