Research At U. Pitt’s New Live Like Lou Center for ALS Research To investigate New Way Of Treating ALS
Written by |

Dr. Christopher Donnelly, PhD, is the first recruit for the University of Pittsburgh Brain Institute’s new Live Like Lou Center for ALS Research. A neurobiologist who co-led a study investigating hexanucleotide repeat expansion (HRE) which scientists say is the most common cause of Amyotrophic Lateral Sclerosis (ALS) and Frontotemporal Dementia (FTD) published recently in the journal Nature, has joined the University of Pittsburgh Brain Institute to continue his scientific efforts at the Live Like Lou Center.
ALS is a rapidly progressive and fatal neurological disease that attacks the nerve cells responsible for controlling muscles. The disease is characterized by progressive muscle weakness, resulting in paralysis. The disease attacks nerve cells in the brain and spinal cord, causing motor neurons, which control movement of voluntary muscles, deteriorate and eventually die. When the motor neurons die, the brain’s ability to initiate and control muscle movement dies along with them, and because muscles no longer receive the messages they need in order to function, they gradually weaken and deteriorate. Some ALS patients retain more limb involvement early on, while those with a bulbar version of the disease will experience difficulty speaking, chewing, and swallowing. Patients in the later stage ALS are totally paralyzed, although their minds remain unaffected. Typically the cause of death from ALS is denervation of the respiratory muscles and diaphragm.
The disease, originally identified by a French physician, Jean Martin Charcot in 1874, is in the the United States commonly referred to as “Lou Gehrig’s Disease” after legendary baseball player Lou Gehrig, who played 17 seasons as first baseman for the New York Yankees and died from ALS in 1941.
Established through the Pittsburgh Foundation by Neil and Suzanne Alexander of Pittsburgh, Pennsylvania suburb O’Hara Township in 2011 soon after Neil was diagnosed with ALS at age 46, the LiveLikeLou.org fund was named for Lou Gehrig to honor the example he set for all people living with ALS. Mr. Alexander died in March, six weeks after creation of the Live Like Lou Center for ALS Research was announced, its mission to develop new treatments, and ultimately, a cure for ALS, and to improve the quality of life for people currently living with the disease.
Currently, only one drug is specifically approved by the FDA for ALS treatment, and therapy is generally limited to supportive care (relieving symptoms, when possible, and addressing quality-of-life issues). Patients with ALS live two to five years, on average, after diagnosis, with roughly 10 percent minority surviving for 10 years or longer. Some 5,600 people in the United States are newly diagnosed with ALS each year (approximately 15 new cases a day) and it is estimated that as many as 30,000 Americans ar living with the the disease at any given time.
Dr. Donnelly has joined the U. Pitt Department of Neurobiology to conduct fundamental research focused on revealing the etiology and pathophysiological mechanisms of action ALS. As a postdoctoral fellow with world-renowned ALS expert Jeffrey Rothstein, MD, PhD, at Johns Hopkins University in Baltimore, Maryland, Dr. Donnelly employed a variety of approaches to revealing the molecular mechanisms that underlie neural injury in ALS and frontotemporal dementia (FTD).
 The Nature study, entitled “The C9orf72 repeat expansion disrupts nucleocytoplasmic transport” (Nature 525, 5661 (03 September 2015) doi:10.1038/nature14973) is coauthored by Dr. Donnell with Ke Zhang, James B. Machamer, Kathleen M. Cunningham, Saksham Gupta, Lyle W. Ostrow, and Thomas E. Lloyd of the Johns Hopkins University School of Medicine Department of Neurology; Jonathan C. Grima, Elizabeth L. Daley, Sean J. Miller, Svetlana Vidensky,Michael A. Thomas, Rita Sattler and Jeffrey D. Rothstein of the Johns Hopkins University School of Medicine Brain Science Institute; Aaron R. Haeusler, Peter Steinwald, Michael J. Matunis, and Jiou Wang of the Johns Hopkins University Bloomberg School of Public Health department of Biochemistry and Molecular Biology; and Ingie Hong, Shu-Ling Chiu, Richard L. Huganir, and Thomas E. Lloyd of the Johns Hopkins School of Medicine Department of Neuroscience.
The Nature study, entitled “The C9orf72 repeat expansion disrupts nucleocytoplasmic transport” (Nature 525, 5661 (03 September 2015) doi:10.1038/nature14973) is coauthored by Dr. Donnell with Ke Zhang, James B. Machamer, Kathleen M. Cunningham, Saksham Gupta, Lyle W. Ostrow, and Thomas E. Lloyd of the Johns Hopkins University School of Medicine Department of Neurology; Jonathan C. Grima, Elizabeth L. Daley, Sean J. Miller, Svetlana Vidensky,Michael A. Thomas, Rita Sattler and Jeffrey D. Rothstein of the Johns Hopkins University School of Medicine Brain Science Institute; Aaron R. Haeusler, Peter Steinwald, Michael J. Matunis, and Jiou Wang of the Johns Hopkins University Bloomberg School of Public Health department of Biochemistry and Molecular Biology; and Ingie Hong, Shu-Ling Chiu, Richard L. Huganir, and Thomas E. Lloyd of the Johns Hopkins School of Medicine Department of Neuroscience.
The investigators conclude that with hexanucleotide repeat expansion (HRE) being the most common cause of ALS and FTD, and recent studies supporting an HRE RNA gain-of-function mechanism of neurotoxicity, nucleocytoplasmic transport defects may be a fundamental pathway for ALS and FTD that may be potentially amenable to pharmacotherapeutic intervention.
The Johns Hopkins research team found that when proteins are made from DNA blueprints, RNA molecules act as a template, with the repeating gene sequence producing RNA that behaves like a sticky spider web and binds other proteins to it, the. In particular, the sticky RNA clog up whats known as the nuclear pore complex, a tunnel-like structure that tightly controls traffic of molecules in and out of the cell’s nucleus.
 As an assistant professor of neurobiology at Pitt School of Medicine, Dr. Donnelly will conduct ongoing research into the HRE pathway and other possible treatment approaches at the Live Like Lou Center.
As an assistant professor of neurobiology at Pitt School of Medicine, Dr. Donnelly will conduct ongoing research into the HRE pathway and other possible treatment approaches at the Live Like Lou Center.
“Pitt is home to renowned scientists and medical practitioners, one of the largest brain tissue research repositories in the world and, most importantly, a strong community that is determined to make a difference in the fight against ALS,” Dr. Donnelly comments in a release. “I am delighted to pursue this work at an institution that has made a profound commitment to treating and hopefully curing this devastating disease.”
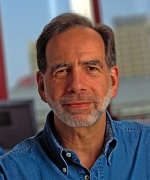 “We are thrilled to have Dr. Donnelly bring his accomplishments and creativity to the Brain Institute,” says Peter Strick, Ph.D. , Pitt’s Dr. Thomas Detre Professor and Chair of Neurobiology and Brain Institute scientific director of the. “His research is taking our understanding of ALS therapeutics in new and promising directions.”
“We are thrilled to have Dr. Donnelly bring his accomplishments and creativity to the Brain Institute,” says Peter Strick, Ph.D. , Pitt’s Dr. Thomas Detre Professor and Chair of Neurobiology and Brain Institute scientific director of the. “His research is taking our understanding of ALS therapeutics in new and promising directions.”
According to Dr. Donnelly, ALS, like cancer, probably has many different causes, making it difficult to find one-size-fits-all solutions. The disease appears to strike randomly, although there is a clear genetic link in a small percentage of cases. “One out of 10 ALS cases is familial and in 40 percent of those we have observed an abnormal repeating gene sequence,” he notes, referencing work he conducted while at Johns Hopkins University. “We wanted to see what proteins that sequence made, so we took skin cells from patients that carried the mutations, converted them into induced pluripotent stem cells and then generated motor neurons for some experiments.”
“One of the hallmarks of ALS is an overabundance of proteins in the cells cytoplasm, Dr. Donnelly observes. “It’s like a car accident in the tunnel is preventing proteins from making their way through to the other side. Eventually, the damaged cells stop functioning and die.”
The Nature study investigators observed that such neurodegeneration was suppressed among Drosophila flies with the gene version of ALS that were given an agent that inhibited the sticky RNA. Another molecule they tested, which acts by altering proteins that control traffic through the nuclear pore complex, also slowed neurodegeneration.
“This pathway could offer us a new way of treating ALS,” Dr. Donnelly suggests. “While there might be different initial triggers of the disease, we suspect many of them might influence the function of this tunnel. We want to further explore this possibility.”
Sources:
Pitt School of Medicine
University of Pittsburgh Brain Institute
Live Like Lou Center for ALS Research
Nature
The Rip Van Winkle Foundation
The Association for Frontotemporal Degeneration
Image Credits:
University of Pittsburgh Brain Institute
The Rip Van Winkle Foundation