Scientists ID site in motor neurons where ALS dysfunction may start
Work may provide new therapeutic target to improve neuronal function
Written by |
Scientists at King’s College London have identified the site in motor neurons that appears to be the starting point of dysfunction in amyotrophic lateral sclerosis (ALS) — shedding new light on the workings of the neurodegenerative disease at its earliest stages.
“This provides a better understanding of the complex mechanism of this disease and a new therapeutic target to improve neuronal function,” Ivo Lieberam, PhD, a study co-author, said in a King’s College news story.
According to the researchers, motor neurons carrying mutations that cause ALS show abnormal activity in a specialized part of the cell called the axon initial segment, which is where electrical signals are started in these nerve cells.
“We showed that the axonal initial segment has an important site of dysfunction in motor neurons caused by different genetic mutations,” Lieberam said.
The study, “Aberrant axon initial segment plasticity and intrinsic excitability of ALS hiPSC motor neurons,” was published in Cell Reports.
Seeking to understand the ‘why’ of changes in ALS motor neurons
ALS is characterized by the death and dysfunction of motor neurons, the nerve cells that control voluntary movement. Normally, motor neurons are activated by signals from the brain, and then send electrical signals down their long, wire-like fibers, known as axons.
When the electrical signal reaches the end of the axon, it prompts the nerve to release signaling molecules to nearby muscle cells, telling the muscle cells to contract.
In ALS, the electrical activity of motor neurons show characteristic abnormalities. In the early stages of the disease, motor neurons are hyperactive, signaling more than usual, which is thought to contribute to ALS symptoms such as muscle twitching. Then, in later stages, motor neurons become hypoactive, with less electrical signaling.
In this study, the team of seven researchers aimed to better understand why ALS motor neurons show these changes in electrical activity. For their experiments, the researchers used patient-derived nerve cells carrying mutations in the TDP-43 or C9ORF72 genes, two of the most common ALS-associated genes.
The researchers noted that, although most cases of ALS don’t have a clear genetic cause, both genetic and non-genetic forms of the disease are typically marked by similar changes in motor neuron activity.
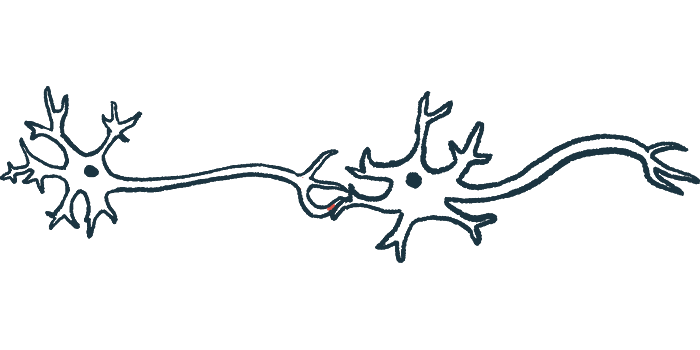
In the early stages of the disease, the scientists found, the ALS motor neurons had abnormally long axon initial segments, or AISs. The AIS is the specific part of the neuron where electrical signals, called action potentials, are started.
“This study has shown us that the AIS is a key site in the early stages of ALS pathology and requires further investigation,” said Juan Burrone, PhD, a co-author of the study and professor at King’s College London.
Normally, the AIS is able to adjust itself, getting longer or shorter to help regulate how often the neuron fires electrical signals. This phenomenon is called plasticity. However, data showed that the AIS had less plasticity in motor neurons carrying ALS-causing mutations — and this lack of plasticity coupled with the abnormally long AIS ultimately caused the neurons to be overactive.
“Our study shows that increased AIS length and impaired AIS plasticity is an important mechanism driving abnormal regulation of neuronal activity and intrinsic hyperexcitability in early ALS,” the researchers wrote.
Further work needed into other types of ALS-causing mutations
In cell experiments in which these motor neurons were coupled with muscle cells, the muscles showed twitches similar to what happens in ALS patients, the researchers noted.
Other experiments indicated that the AIS also was dysregulated in later stages of the disease, where it was abnormally short — contributing to reduced activity of the motor neurons. Consistent with these experiments in cell models, analyses of tissue from people who had died from ALS also were indicative of a shortened AIS in the latter stages of the disease.
“Taken together, our findings point toward an important and dynamic role of the AIS as a site of dysfunction in ALS [motor neurons],” the scientists concluded.
The team highlighted that this study was limited to cells carrying only two types of ALS-causing mutations, so further work will be needed to determine whether these findings are applicable in all forms of the disease.
Taken together, our findings point toward an important and dynamic role of the AIS [axonal initial segment] as a site of dysfunction in ALS [motor neurons].
Also, further work is needed to understand exactly how AIS abnormalities in motor neurons may alter the activity of other nerve cells and muscle cells that normally interact with motor neurons, the team noted.
“We now need to expand our investigation across other spinal cord and brain regions and different genetic mutations,” Burrone said.
“It will be important to examine whether these structural and molecular changes of the AIS destabilise the neurons somehow, rendering them vulnerable to further pathological insults,” he said.