SOD1 Enzyme Clumps May Expose Cells to DNA Damage in Some ALS Patients, Study Suggests
Written by |
The enzyme superoxide dismutase 1 (SOD1) forms clumps inside the cells of some people with sporadic amyotrophic lateral sclerosis (ALS), making them more vulnerable to DNA damage — which may contribute to the neurodegeneration that marks the disease, an early study suggests.
In other patients, SOD1 is transported to the cell nucleus, where it enhanced DNA protection. These findings hint that targeting the cell nucleus may be a promising therapeutic strategy to explore in the future, the researchers said.
Their study “Nuclear Phospho-SOD1 Protects DNA from Oxidative Stress Damage in Amyotrophic Lateral Sclerosis” was published in the Journal of Clinical Medicine.
Mutations in the SOD1 gene account for 12-20% of familial ALS cases, and about 1% of sporadic ALS, in which the cause of the disease is unknown.
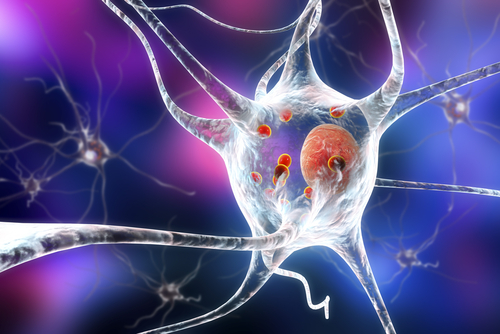
This gene provides instructions for the production of superoxide dismutase 1 (SOD1), an enzyme that binds to copper and zinc molecules to neutralize toxic oxygen radicals — called superoxide radicals — that form as a byproduct of normal cell processes.
However, how these alterations in SOD1 lead to the death of motor neurons and cause ALS is not well understood.
Some researchers believe SOD1 defects may leave cells unprepared to repair DNA damage, making them more susceptible to dying due to the superoxide radicals.
Consistent with this hypothesis, there is evidence that DNA repair pathways, and the DNA damage response (DDR), are impaired in many neurological disorders, including ALS.
Genome stability is fundamental for cells’ survival, especially in nerve cells, which are particularly prone to DNA damage — through DNA breaks or oxidative stress — due to their high metabolic rates, the investigators said.
In a prior work, the researchers saw that SOD1 could form aggregates, or clumps, inside peripheral blood mononuclear cells (PBMCs) — which consist of blood cells without red blood cells and platelets — of sporadic ALS patients who did not carry a SOD1 mutation.
Another study went further and distinguished two groups of patients — those who accumulated SOD1 aggregates inside the cell’s cytoplasm, the solution filling in most of the cell; and those in whom SOD1 relocated to the nucleus, the cell compartment enclosing the DNA.
To better understand the role of SOD1 in ALS, the researchers investigated the differences — in particular, regarding DNA repair — between PBMCs collected from these two distinct groups of patients.
Recent evidence suggests that non-neural cells like PBMCs also could trigger motor neuron death, supporting their use for studying neurodegeneration.
A DNA damage assay revealed that PBMCs from patients with high levels of nuclear SOD1 were protected against DNA damage, much like cells from healthy controls.
In contrast, PBMCs from people with insoluble aggregates of cytoplasmic SOD1 had extensive DNA damage.
“This finding confirms our hypothesis that normal soluble SOD1 could have a potential protective role in DNA damage mediated by oxidative stress,” the researchers said.
Researchers reasoned that clumped SOD1 was not working, thus leading to an increase of oxidative stress. Conversely, SOD1 that translocates, or moves to the nucleus could remain functional and protect DNA from oxidative damage.
The team tested this possibility in a nerve cell model that was treated with hydrogen peroxide to increase its exposure to oxidative stress.
They found that a higher concentration of SOD1 in the nucleus had a protective role in the DNA damage mediated by oxidative stress. On the contrary, when SOD1 is forced into the cytoplasm, it cannot protect DNA from damage.
The researchers also uncovered a modification — a phosphorylation of SOD1 — which could serve as the ‘shuttle’ signal to move the enzyme from the cytoplasm to the nucleus to help protect DNA.
“These data should open a new scenario into the development of new therapies of ALS, in particular targeting molecules involved in oxidative stress protection,” the researchers said.
“As yet to reported in cancer research, the nucleus could be a persuasive drug target, in particular by delivering nanoparticles directed in the proximity of the nucleus or against the nucleus itself. Targeted drugs that can reduce oxidative stress damage can have a pivotal role in delay the progression of the pathology,” they concluded.