Stem Cell Treatment Targeting Spinal Cord Won’t Slow ALS, Researchers Say
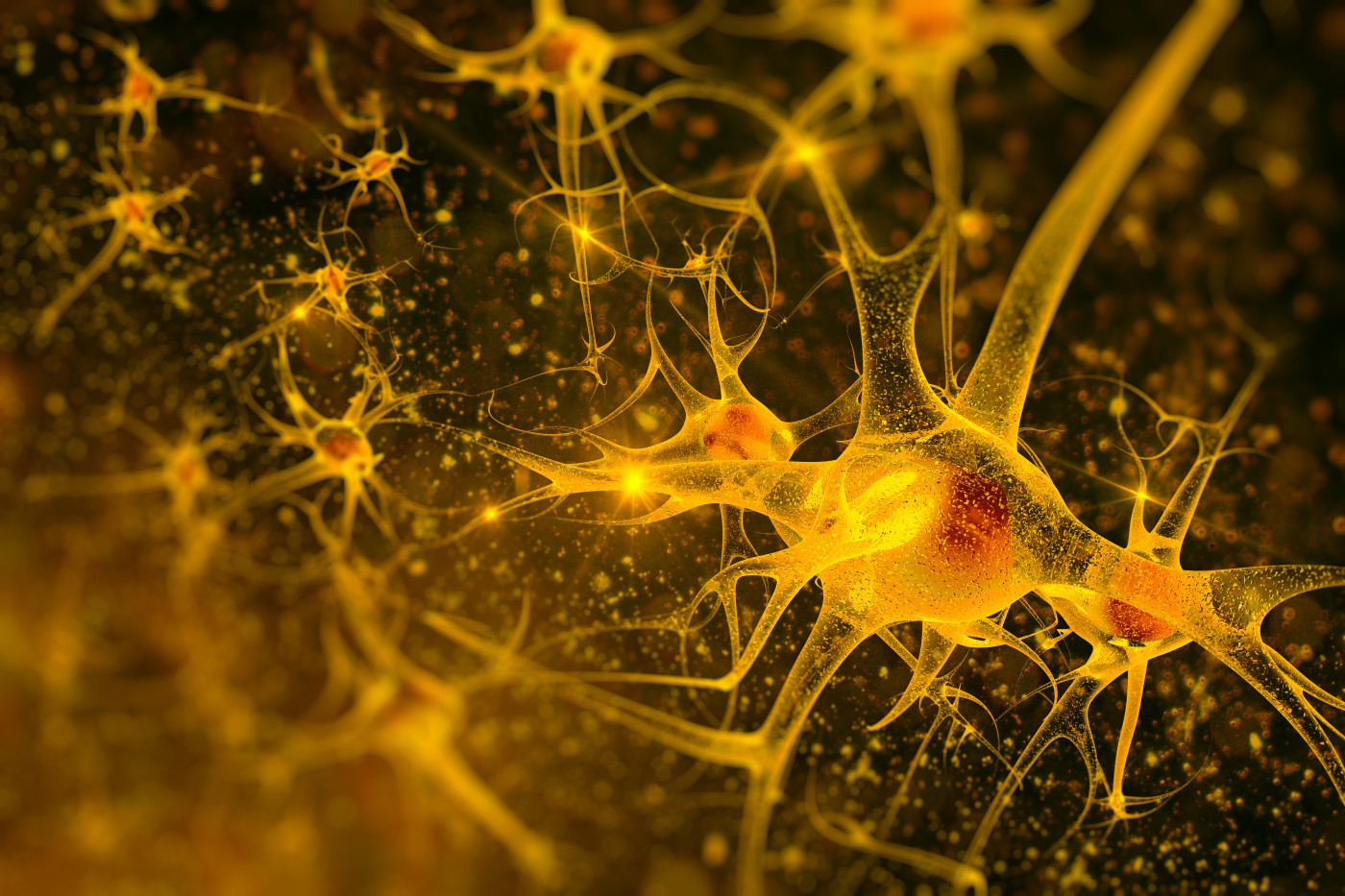
Using stem cell treatments to protect motor neurons is not enough to prevent the loss of nerve-muscle connections and disease progression in a mouse model of amyotrophic lateral sclerosis (ALS), researchers from Italy found.
The study, published in the journal Stem Cell Research, had exposed mice to repeated brain injections of so-called mesenchymal stem cells, gathered from the umbilical cord. But, while the cells lessened inflammation in the spinal cord, it became apparent that more is needed to slow disease progression.
Earlier studies had noted that treatment with mesenchymal stem cells could improve survival in genetic ALS mouse models if started at birth or before symptoms appeared. But since human patients do not receive treatment until the disease is apparent, researchers at the Mario Negri Institute for Pharmacological Research in Italy wanted to test the approach in mice with obvious disease signs.
For the study, “Multiple intracerebroventricular injections of human umbilical cord mesenchymal stem cells delay motor neurons loss but not disease progression of SOD1G93A mice,” they gathered mesenchymal stem cells from human umbilical cords.
They injected them into the mice brain ventricles, which are natural fluid-filled cavities in the brain. The animals received injections once every two weeks — getting a total of three injections.
The team had hoped that the cells would travel to the spinal cord, but results were disappointing. Nonetheless, it became apparent that the cells did impact the environment in the spinal cord even from their position in the brain ventricles.
Researchers noted that the environment in the spinal cord shifted from a pro-inflammatory to an anti-inflammatory state — evident by changes in immune mediators called cytokines. Changes also were seen in the activity of glial cells involved in spinal cord inflammation.
Meanwhile, protective molecular pathways, acting to prevent cell death, had been activated in the mice spinal cords. While the cells did not reach the spinal cord, researchers said the effects indicated they secreted factors that could impact processes in other parts of the central nervous system.
Despite this protective environment, with more motor neurons surviving in the spinal cord, motor neuron axons were disconnected from the muscles and the team noted no slowing of disease progression. While not statistically significant, they did note a slight increase in survival time, however.
The findings suggest that potential stem cell or other neuro-protective treatments — delivered into the central nervous system —need to be combined with approaches that protect the connection between motor neurons and muscles to prevent disease progression.