Fungus Used in Chinese Medicine Reduces Motor Neuron Loss and Prolongs Life in Mouse Model of ALS, Study Shows
The Chinese caterpillar fungus (Hirsutella sinensis), used in traditional Chinese medicine, minimized motor neuron loss and extended the lifespan in a mouse model of amyotrophic lateral sclerosis (ALS), a study has found.
The study, “Therapeutic effects of hirsutella sinensis on the disease onset and progression of amyotrophic lateral sclerosis in SOD1G93A transgenic mouse model,” was published in CNS Neuroscience & Therapeutics.
ALS is a progressive neurodegenerative disorder caused by the gradual destruction of motor neurons — nerve cells responsible for voluntary muscle control — in the spinal cord and brain.
Although the molecular mechanisms underlying the development and progression of ALS are not fully understood, scientists believe a group of nerve cells called microglia, which are normally responsible for protecting and supporting neurons, may become overactive and stimulate the brain inflammation associated with ALS.
“Hirsutella sinensis (HS) is a unique fungus growing on caterpillars and is a highly valued tonic medicine claimed to treat a wide range of disorders, such as asthma, chronic kidney disease, and kidney transplant recipients,” the researchers wrote. “Cordycepin (3′‐deoxyadenosine), one of the major chemical components of HS, has been identified to exert anti‐oxidative, anti‐inflammation, antitumor, and neuroprotective effects. Moreover, previous studies have further revealed a suppressive role of cordycepin on (…) microglia activation and inflammation in vitro.”
Therefore, a group of researchers from the Dalian Medical University in China set out to assess whether treatment with HS might reduce signs of neuroinflammation in mice with ALS.
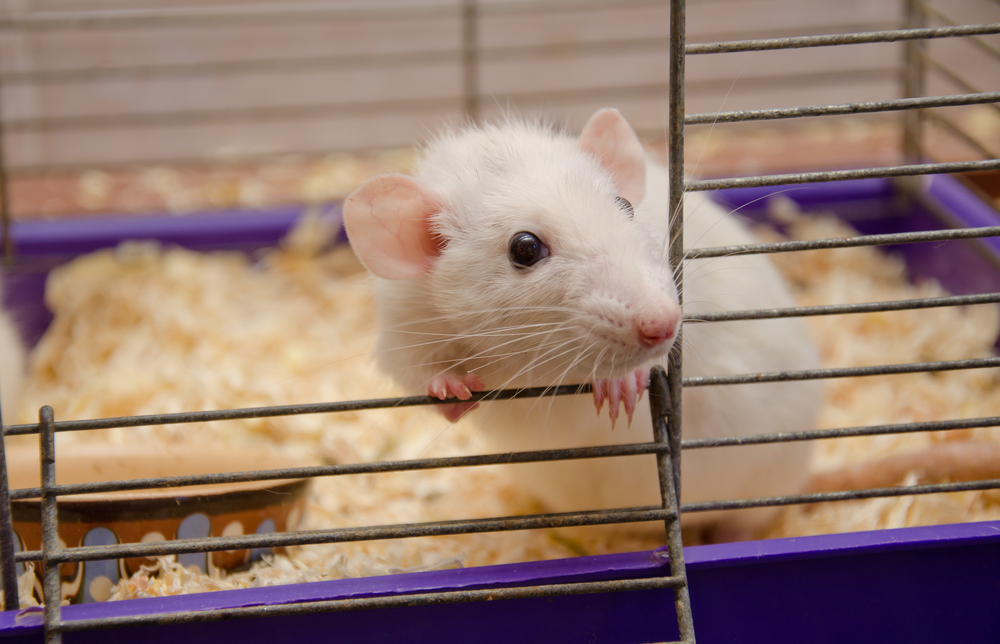
To test their hypothesis, the researchers administered HS to animals with ALS (SOD1G93A mice) by gavage (a technique in which the medication is deposited directly into the animal’s stomach using a long probe that is inserted in the mouth).
A total of 28 mice were randomly selected to receive a daily gavage containing HS (1 g/kg body weight, 10 mL/kg), and another 28 to receive a daily gavage containing drinking water (10 mL/kg body weight, controls).
The lifespan of all animals was recorded, and the rotarod test, a test in which animals must stay on a rotating rod for at least five minutes, was used to assess their motor function.
Imaging techniques were used to visualize morphological alterations in the animals’ muscles and spinal cord motor neurons caused by ALS. Immunofluorescence and quantitative real-time polymerase chain reaction (qRT-PCR, a technique to measure the expression levels of genes) were used to assess microglia activation and neuroinflammation.
The results showed that despite developing ALS roughly at the same time (day 104.1 for HS-treated mice versus day 99.3 for controls), mice that had been treated with HS lived longer (143.7 days) than those that had been treated with drinking water (126.8 days).
Moreover, repeated treatment with HS also prolonged disease duration (39.6 days for HS-treated mice versus 27.7 days for controls), which is time between the day of disease onset and the day of death.
In addition, the investigators found that HS treatment reduced the loss of spinal cord motor neurons associated with ALS progression (7.70 motor neurons/slide in HS-treated mice versus 18.0 motor neurons/slide in controls), as well as morphological changes in muscle fibers of leg muscles associated with disease progression (muscle atrophy, or shrinkage).
Finally, they also found that repeated HS treatment stimulated microglia in the spinal cord of ALS mice to shift their state from “pro-inflammatory active” to “anti-inflammatory stable.”
“The therapeutic effects of HS against ALS might be mediated by its activities of anti‐oxidative stress [cellular damage that occurs as a consequence of high levels of oxidant molecules] and anti‐inflammation through promoting transition of microglia polarization from [an active to stable state]. All these findings predicted a promising therapeutic potential of HS for ALS,” the investigators wrote.