Researchers Identify New Genetic Defect Linked to ALS
Mutations in the UBQLN2 gene, known to cause amyotrophic lateral sclerosis (ALS), promote the buildup of toxic waste in brain cells by preventing the normal function of two cellular degradation mechanisms, a study has found.
In addition to its known role in the proteasome, a mechanism used for clearing out abnormal proteins, the UBQLN2 protein also is needed for autophagy, another recycling mechanism used to eliminate larger components of cells, including the toxic protein aggregates seen in ALS patients.
The study, “ALS/FTD mutations in UBQLN2 impede autophagy by reducing autophagosome acidification through loss of function,” was published in PNAS.
Mutations in UBQLN2, which carries the information to produce the ubiquilin 2 (UBQLN2) protein, are known to cause ALS. But the exact mechanisms through which these mutations contribute to disease are not fully understood.
Studies have demonstrated that UBQLN2 is involved in protein quality control, helping cells degrade faulty components and helping proteins acquire their normal 3D structure.
Mutations in UBQLN2 are known to affect how cells clear out toxic waste via the proteasome. While signs exist that autophagy also is dampened, evidence is “more circumstantial,” the researchers wrote.
A team at the University of Maryland School of Medicine (UMSOM) set out to investigate whether these mutations also contribute to ALS by impairing the autophagic process, and exactly how this mechanism is affected.
Using human cells and animal models carrying known disease-causing mutations in UBQLN2, the team found that autophagy was completely stalled when UBQLN2 was not working properly. While reintroducing a normal UBQLN2 gene into cells was able to restore this recycling mechanism, none of the five different UBQLN2 mutants restored the autophagic pathway.
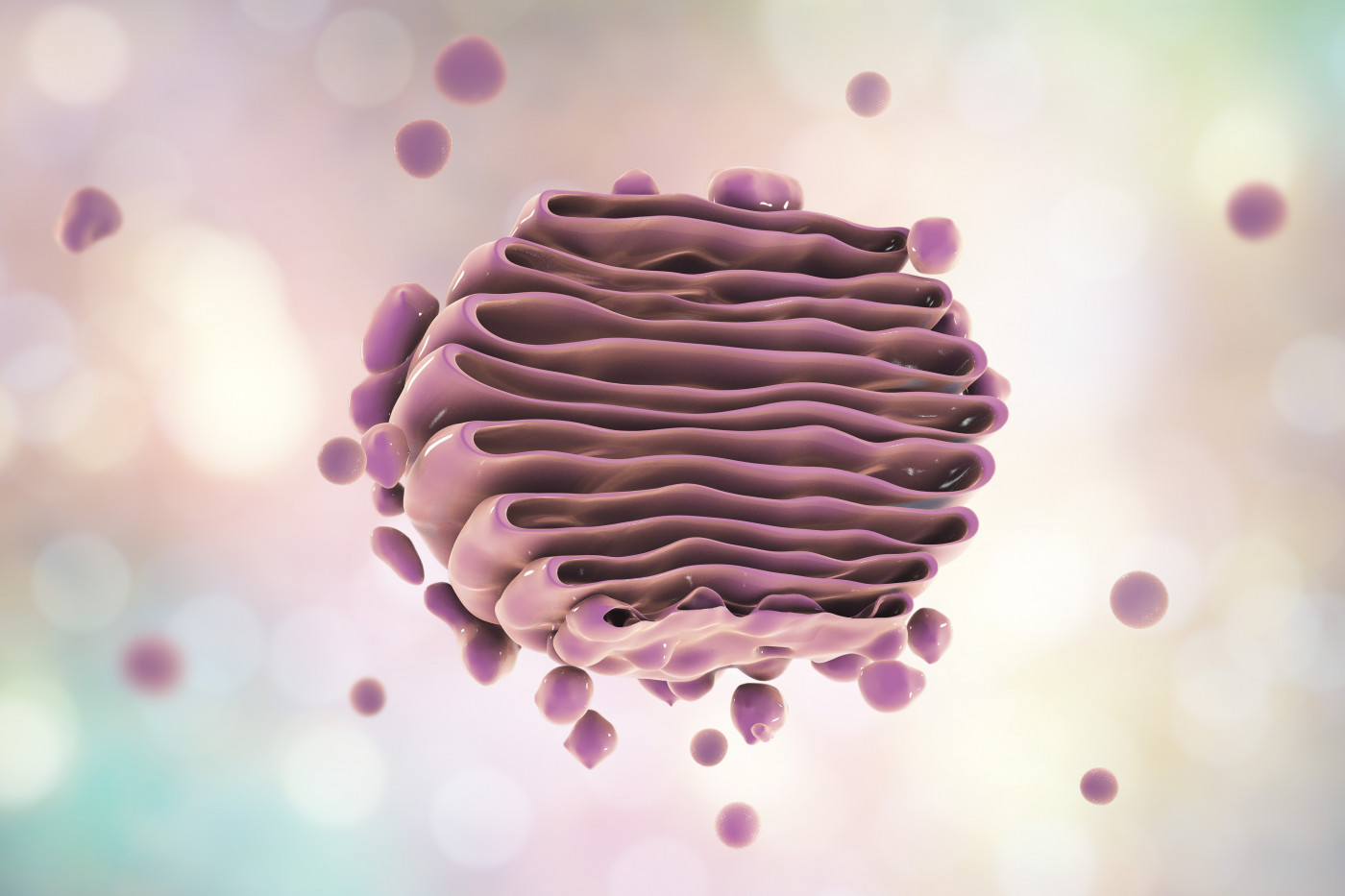
Autophagy is a degrading process in which vesicles containing cellular trash, called autophagosomes, are fused with another cellular component called the lysosome. Autophagosomes are very acidic (have a very low pH), and lysosomes carry proteins that degrade the toxic components under these acidic conditions.
But the mutations in UBQLN2 caused a loss of acidification in these vesicles, ultimately preventing the lysosomal proteins from clearing out the toxic waste.
The researchers then found that the defects in acidification were caused by the loss of another protein called ATP6v1g1, which is a critical subunit of the pump that regulates vesicle acidification and is essential for autophagosome maturation.
While this protein is degraded by the proteasome, the researchers did not think the lower levels of ATP6v1g1 were due to problems in this recycling process. Rather, they found that UBQLN2 was needed for ATP6v1g1 to fold adequately, and that the mutated protein had much lower affinity to ATP6v1g1 than the normal protein.
“Mechanistic insight into the underlying reason for the reduction in ATP6v1g1 levels suggests a likely role of UBQLN2 as a chaperone in binding and facilitating ATP6v1g1 biosynthesis,” the researchers wrote.
Notably, increasing the expression of ATP6v1g1 in cells lacking the UBQLN2 protein was able to restore the autophagosome acidification, suggesting a possible mechanism to ease symptoms of ALS patients carrying these mutations.
“Our new findings are exciting because similar acidification defects have been found in Alzheimer’s, Parkinson’s and Down syndrome,” Mervyn Monteiro, PhD, professor of anatomy and neurobiology at UMSOM, said in a press release. “This suggests that restoration of the defect could have broad implications for not only treating ALS, but possibly other neurodegenerative diseases as well.”






