Insurance and financial resources for ALS treatment
Last updated June 17, 2024, by Susie Strachan
Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive, neurodegenerative condition resulting in muscle weakness and other symptoms. Financial planning can help with managing expenses related to living with ALS so you can focus on your health and well-being.
Working with a financial adviser or navigator can help with finding health insurance for people with ALS, along with state and federal financial assistance programs.
Cost of ALS

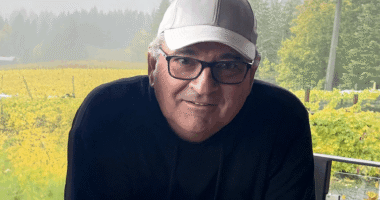
Kara Nett Hinkley is the vice president of state policy with the ALS Association. (Photo courtesy of Kara Nett Hinkley.)
Kara Nett Hinkley, vice president of state policy with the ALS Association, says people with ALS can pay between $80,000 and $250,000 a year out of pocket for care and ALS treatment.
“In that amount, you’re having health insurance deductibles, co-payments, medications, and what you’re paying at the pharmacy counter,” she says.
In addition, people with ALS have expenses for mobility aids, modifications to their home, in-home care, hospital stays, and other ALS supports.
You also may be dealing with indirect costs, such as lost income from leaving the workforce yourself and a family member if they become your caregiver.
“If they have private insurance through their employer and then they end up on Medicare, how does that impact the family’s insurance coverage?,” she says. “And, most folks, they’re diagnosed with ALS around the age of 55. At that point, you may still have children that were on your employer-sponsored coverage. And from there on, that all rolls downhill.”
Planning your financial future
As ALS can vary, getting your financial affairs in order can take on some urgency, according to Nett Hinkley.
Financial counseling can start soon after being diagnosed, along with other important conversations you are probably having. This might include talking about the benefits of early intervention, better home accessibility, setting up medical directives, and undergoing genetic testing and counseling.
Nett Hinkley says there are numerous financial questions related to your health you want to address, such as:
- What health insurance should you get?
- What life insurance can you get?
- Can you stay on your employer-sponsored health insurance plan?
- Will you need to go on social assistance such as Medicaid?
- If you are a veteran, how can you qualify for Department of Veterans Affairs assistance?
- Should you set up a power of attorney for handling your finances?
- Should you set up a living trust for passing on your financial assets to your family?
“As you can see, financial decisions are colored by your healthcare decisions pretty quickly,” she says.
Consider consulting a financial planner who specializes in chronic illness. They can guide you through your financial options to cover your medical expenses and the other costs of daily living with ALS.
The ALS Association and the Patient Advocate Foundation have an ALS insurance and benefits resource line.
Financial navigators can help you with eligibility and enrollment in disability benefits, insurance coverage, prescribed and emerging ALS therapies, and other financial issues associated with the disease.
For more information, contact the ALS Association at 1-844-244-1306.
Health insurance
Health insurance in the U.S. can be complicated and may leave you feeling frustrated and overwhelmed.
If you are changing your insurance, you want to do your best to find health insurance that covers your ALS medications, treatments, and other healthcare services. Look for insurance that doesn’t have coverage gaps, high out-of-pocket expenses, and inconsistent access to healthcare providers.
According to Nett Hinkley, the financial and insurance navigators at the ALS Association have seen cases where a person with ALS makes multiple appeals to get the care they were prescribed.
To learn what a health insurance plan does or does not cover for people with ALS, there are some questions you can ask. For example, will the plan cover:
- all Food and Drug Administration-approved ALS drugs or only from its list of drugs (formulary)
- durable medical equipment and is there a preferred provider
- private nursing or a healthcare aide at home
- ALS specialists from the plan’s participating providers.
Nett Hinkley notes that getting your ALS medical needs met should not be affected by health insurance limitations.
“Doctors’ orders should be followed, such as when a doctor prescribes a therapy or a device,” she says. “That person who has health insurance should be able to get what they are prescribed.”
Nett Hinkley points out two other potential pitfalls related to insurance coverage that can prove to be barriers to starting or continuing ALS treatments.
The first is pharmacy benefit managers. These are intermediaries in the healthcare system who create and manage lists of covered medications on behalf of health insurers, Medicare Part D drug plans, large employers, and other payers.
“One of the biggest things I’m always telling people to do when they’re denied a prescription, when they’re denied durable medical equipment that has been prescribed, is to go to their state insurance commissioners’ website and file a complaint,” she says. “Every single time.”
In 2024, an analysis of clinical practices found that while guidelines for treating ALS recommend three available treatments be given together, the majority of people with ALS are not receiving this kind of treatment, possibly due to issues with health insurance.
The second insurance pitfall is in the area of genetic testing, which many people with ALS undergo to determine if they have the familial or sporadic form of the disease. Identifying specific genetic causes also can guide treatment. People with certain genetic mutations may be eligible for specific clinical trials.
In 2020, Florida became the first U.S. state to prohibit the use of genetic information to deny coverage by life, long-term care, and disability insurers. Several other states have enacted similar protections to prevent discrimination based on genetic information.
“Folks are talking about genetic testing and genetic counseling. Unfortunately, because there aren’t those genetic testing protections in the majority of states, if folks do that before getting a life insurance policy, they may not be able to get one,” Nett Hinkley says.
She says her team is keeping an eye on the rise of the use of artificial intelligence in the health insurance field.
While artificial intelligence has the potential to connect ALS patients with clinical trials and other benefits, it also is playing a role in the number of healthcare insurance claim denials, according to Nett Hinkley.
“Things are happening in a black-box algorithm that nobody has the code to, that consumers can’t understand,” she says.
On a positive note, by 2024, at least eight U.S. states will have created drug affordability boards to regulate the prices of prescription medications, including essential ALS medications, to ensure they remain affordable for consumers, she says.
Assistance programs
In the U.S., assistance programs are another financial resource for ALS.
Among these are:
- federally run Social Security Disability Insurance (SSDI), Medicare, and Medicaid programs
- state-run programs that offer additional financial support, including Medicaid
- Veterans Affairs health benefits for veterans diagnosed with ALS
- nonprofit associations that offer grants and financial assistance.
Nett Hinkley leads the state policy team at the ALS Association, which does regulatory and legislative work throughout the U.S. with the goal of improving the benefits for all people living with ALS.
“One of our biggest wins more recently has been in Kentucky in 2023, getting Medigap expanded so that it helps those who are living with ALS who qualify for SSDI and are enrolled in Medicare,” Nett Hinkley says.
Medigap, also known as Medicare supplement health insurance, helps cover some of the healthcare costs that original Medicare (Part A and Part B) does not cover, such as copayments, coinsurance, and deductibles. It also may cover expenses that would otherwise come out of pocket, such as emergency medical care during foreign travel, or traveling to clinical trials.
“If your medical costs are $250,000 a year, you can only imagine that the 20% not covered by traditional Medicare isn’t doable for most people,” she says. “If you’re able to buy a Medigap plan at an affordable rate, it will cover that 20%. For people living with ALS, they want to be able to buy these plans to protect their families.”
State assistance programs
Many U.S. states have programs that offer financial aid, medical assistance, and support for home modifications and assistive devices for people with ALS. Some states also have programs to help residents afford prescription medications, which are often a significant expense for people with ALS.
To find state-sponsored ALS financial assistance programs, start by contacting your state’s department of health or human services. Your local ALS clinic or healthcare team may also be able to direct you to financial assistance programs.
Community assistance programs
Charitable organizations offer grants and financial assistance programs to help cover costs not covered by health insurance, such as respite care, home modifications, and durable medical devices.
The following organizations offer financial assistance in the form of grants to people living with ALS:
- Les Turner ALS Foundation Grants & Equipment Assistance (to qualify, you must attend the Lois Insolia ALS Clinic at Northwestern Medicine)
- ALS Association financial assistance grants (state chapters offer grants and financial aid programs to help cover costs such as home modifications, equipment, and caregiving)
- Muscular Dystrophy Family Foundation financial assistance
- Patient Advocate Co-pay Relief Program for ALS
- Needymeds (maintains a list of financial assistance resources for people with ALS)
- HealthWell ALS Premium Assistance fund
- Project Main Street financial help fund.
For current and specific financial assistance information, contact your state health department or your local ALS association directly.
ALS News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.